Received: Fri 01, Sep 2023
Accepted: Tue 26, Sep 2023
Abstract
Background: Blast injuries are similar to any other burn injuries. Emphasis is given to safety measures as the treatment of burns is a painful and prolonged process that involves a loss of limb or sensory organs with a lot of expenditure. Aim: To evaluate the patient with their outcomes and management who sustained blast injuries. Patients and Methods: All patients who had blast injuries with different kinds and mechanisms were prospectively studied and clinical presentation, management and outcomes were reviewed. Results: 6 patients were studied with different age groups and different mechanisms of blast injuries of which one was female who sustained thermal injuries associated with AC Blast, two patients sustained explosive blast, and others were involved in methanol cylinder blast, improvised explosive device and mixing fertilizer as a chemical form of blast injuries respectively. All were managed and the outcome was satisfactory for 2 individuals, 3 sustained amputations and 1 sustained mortality. Conclusion: The high energy wave produced during blasts are strong enough to produce fatal injuries that will lead to high morbidity and mortality. Civilians should be aware and personal protective equipment should be worn by those who are indulged in this hazardous occupation.
Keywords
Blast injuries, amputation, improvised explosive devices, thermal burn injuries
1. Introduction
Blast injury explosions are very devastating injuries which affect various systems and increase morbidity and mortality similar to any other traumatic injuries. Explosions can occur due to chemical reactions and generate more intense energy and cause damage, it can be in various forms like primary, secondary, tertiary and quaternary. The pattern of injuries following blasts is a product of the composition and amount of the chemical or material used, the surrounding area, the delivery method, the distance between the source and the victim, and any intervening protective barriers or environmental hazards. Explosions are relatively infrequent but very devastating, many of them are associated with head injury, thermal burn injuries, extremities injury and sometimes mortality can occur. Blast-related injuries can present unique triage, diagnostic, and management challenges to provide emergency care [1-4]. According to triage patients are managed accordingly.
2. Case Series
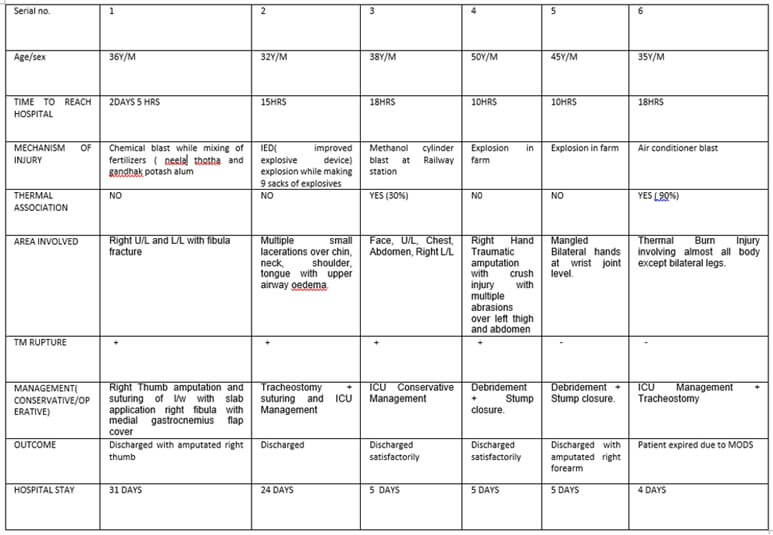
All patients who had blast injuries with different kinds and mechanism were prospectively studied and clinical presentation, management and outcomes were reviewed. Six patients were studied with different age groups and different mechanisms of blast injuries out of which one patient was female who sustained thermal burn injuries associated with AC Blast, two sustained explosive blasts, one each with methanol cylinder blast, improvised explosive device and mixing fertilizer as a chemical form of blast injuries respectively. Clinical course and outcome of patients shown in (Figure 7).






3. Discussion
Blast injuries are more dangerous because when explosion occurs, high energy produce and causes much more damage than other injuries and affects on multisystem of body. If blast injury occur in enclosed space it increase morbidity and mortality [5-7]. In blast various manner of injuries occur and classified into four types primary, secondary, tertiary, and quaternary (Figure 8).
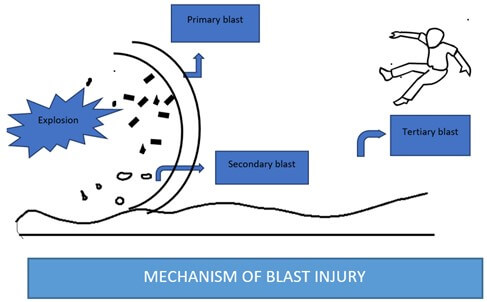
3.1. Primary
It occurs due to direct effect of explosion and effects various vital organs like eye, ear, nose, abdomen, extremities, lung, heart and brain. Perforation and vision loss can occur in eyes, tympanic membrane perforation, hearing loss can occur in ear, internal haemorrhage and compartment syndrome can occur in the abdomen, bleeding can occur in the nose, amputation can occur in both extremities, barotrauma can occur in lungs, cardiac tamponade can occur in heart, parenchymal damage can occur in the brain.
3.2. Secondary
Secondary damage can occur due to the production of debris after an explosion. It causes lacerations over the face, neck, extremities and various parts of the body.
3.3. Tertiary
It occurs due to a displaced object via air and colloids to other objects and causes fatal injury and may cause death.
3.4. Quaternary
It includes all types of injuries which are not included in primary, secondary and tertiary. It occurs in various manners if an explosion and fire occur in an enclosed space it causes thermal burn and inhalational injury. If inhalation injury occurs in COPD and asthma patients it increases morbidity and mortality. Some toxins are also produced after an explosion and cause toxaemia. In myocardial ischemic patients, blast injury precipitates cardiac events like arrhythmia, MI, heart failure etc.
A blast is a high-energy explosion, it occurs due to any cylinder blast, chemical explosion, bomb blast and etc. If the patient survives after a blast injury its effects long term like disability, phantom limb pain, depression, vision loss, sleep disorder, anxiety, psychological disturbances and overall decreased quality of life. In blast injury, patients manage accordingly to protocol (Figure 9).
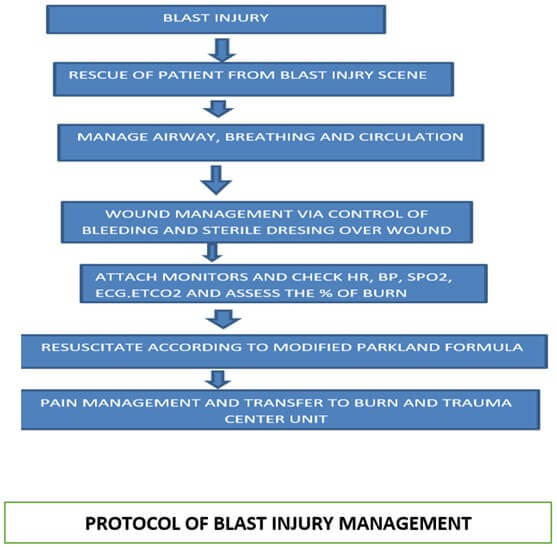
On arrival to burn and trauma unit, take proper history of deafness, vision loss, hemoptysis, abdominal distension, guarding and rigidity, tinnitus, any bleeding from nose and ear, nausea, cough, any respiratory distress do chest x ray, ABG, abdominal x ray or CT scan, ophthalmology consultation and managed accordingly.
4. Conclusion
The high energy wave produced during blasts are strong enough to produce fatal injuries that will increase morbidity and mortality. People should be aware and personal protective equipment should be worn by those who are indulged in this hazardous occupation.
Funding
None.
Conflicts of Interest
None.
REFERENCES
[1] Sule
Temizkan, Fahrettin Kelestimur “A clinical and pathophysiological approach to
traumatic brain injury-induced pituitary dysfunction.” Pituitary, vol.
22, no. 3, pp. 220-228, 2019. View at: Publisher Site | PubMed
[2] Sabri
T Shuker “Emergency Treatment of Blast, Shell Fragment and Bullet Injuries to
the Central Midface Complex.” J Maxillofac Oral Surg, vol. 18, no. 1,
pp. 124-130, 2019. View at: Publisher Site | PubMed
[3] Gregory
T. Guldner; Curtis Knight “Napalm Toxicity.” StatPearls [Internet],
2022. View at: PubMed
[4] Dilaver
Singh, Duane Cronin “Multi-Scale Modeling of Head Kinematics and Brain Tissue
Response to Blast Exposure.” Ann Biomed Eng, vol. 47, no. 9, pp.
1993-2004, 2019. View at: Publisher Site | PubMed
[5] Marek
Dokoupil, Klára Marecová, Matěj Uvíra,
et al. “Fatal delayed
hemopericardium and hemothorax following blunt chest trauma.” Forensic Sci Med Pathol, vol.
15, no. 2, pp. 272-275, 2019. View at: Publisher Site | PubMed
[6] Meghan E Robinson, Ann C McKee, David H Salat, et al. “Positron emission tomography of tau in Iraq and Afghanistan Veterans with blast neurotrauma.” Neuroimage Clin, vol. 21, pp. 101651, 2019. View at: Publisher Site | PubMed
[7] Gilles Van Haesendonck, Vincent Van Rompaey, Annick Gilles, et al. “Otologic Outcomes After Blast Injury: The Brussels Bombing Experience.” Otol Neurotol, vol. 39, no. 10, pp. 1250-1255, 2018. View at: Publisher Site | PubMed
