Received: Fri 02, May 2025
Accepted: Tue 03, Jun 2025
Abstract
Schwannoma is a painless, benign, and slow-growing tumor of the peripheral nerve sheath. About 25-50% of schwannomas occur in the head and neck region, and tumors originating from the nasal cavity or paranasal sinuses are rare. This article reports a case of a patient who underwent endoscopic nasal resection for a tumor in the sphenoid sinus. During the surgery, the internal carotid artery ruptured for unknown reasons. After packing and hemostasis, a Willis covered stent was used to isolate the blood flow. Subsequently, cranial base reconstruction was performed. The patient recovered well after the surgery and showed no signs of recurrence. This article details the emergency treatment of internal carotid artery rupture during the surgery and the subsequent recovery of the patient. Through this case, the aim is to summarize the experience in dealing with internal carotid artery rupture during surgery, provide a reference for the management of vascular accidents in neurosurgery, and enhance the safety and effectiveness of neurosurgical operations.
Keywords
Emergency treatment, schwannoma, surgery, rupture of internal carotid artery
1. Case Information
1.1. Medical History
The patient is a 38-year-old female who was admitted to the hospital on June 25, 2024, with the chief complaint of “headache, dizziness, and nausea for 7 days”.
1.2. On Admission Physical Examination
No abnormalities were found except for limited abduction of the right eye.
1.3. Auxiliary Examinations
Pituitary function tests: sex hormone series: normal, thyroid series: normal, cortisol rhythm, adrenocorticotropic hormone rhythm: normal; visual acuity, visual field, fundus examination were all normal; head MRI plain scan and enhanced scan suggested: Tumor in the left nasal cavity, sphenoid sinus and maxillary sinus, nature unknown (Figures 1A-1C).
1.4. The Treatment Process
A systematic and detailed preoperative assessment was conducted. Preoperative plans were made comprehensively for various possible situations during the operation. The endoscopic sinus tumor resection was performed.
After complete resection of the tumor during endoscopic surgery, it was found that the inner wall of the left cavernous sinus was missing, the internal carotid artery was exposed, and the adventitia of the local internal carotid artery was invaded by the tumor, with bleeding from the wound surface. The bleeding gradually evolved into hemorrhage, and then about 2000 ml of blood was sprayed out instantaneously (Figure 1D). Hemostasis with hemostatic materials was ineffective, and immediate packing with iodoform gauze strips successfully stopped the bleeding (Figure 1E). At the same time, a full-brain angiography was performed, which confirmed the rupture and hemorrhage of the cavernous segment of the left internal carotid artery (Figure 1F). Under the guidance of a microcatheter and a microguidewire, the microcatheter was advanced to the middle cerebral artery to confirm that the guidewire was in the true lumen. A 3.5-16 intracranial covered stent system was gradually released at the rupture site, and the covered stent was delivered to the appropriate position along the microguidewire (Figure 1G), with the distal end reaching the opening of the ophthalmic artery, covering the rupture site, and the stent was released by inflating the balloon with appropriate pressure.
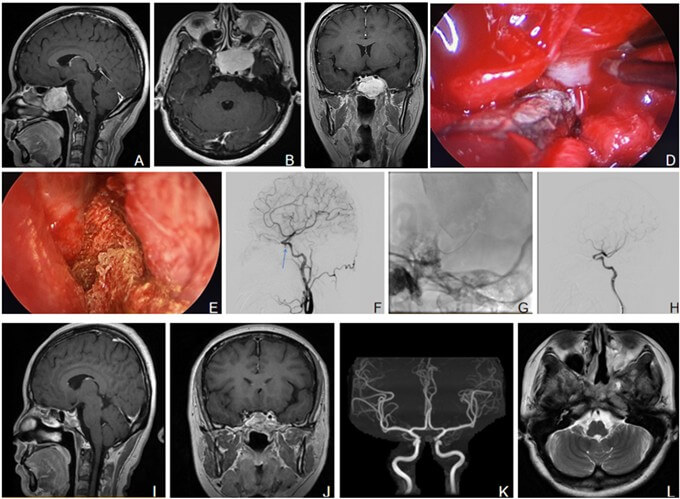
A-C) Preoperative plain and enhanced MR images of the head of the patient (the tumor is closely related to the left internal carotid artery cavernous segment). D-E) Endoscopic surgery (D: The internal carotid artery ruptured and bled in a jet-like manner. E: Temporary packing to compress and stop bleeding). F-H) Left internal carotid artery angiography and stent implantation (F: The angiography showed a rupture of the cavernous segment of the internal carotid artery and extravasation of contrast agent. G: The stent is in place. H: Postoperative angiography shows no extravasation of contrast agent at the rupture site). I-J) A reexamination of the cranial MRI half a year after the operation shows no recurrence of tumors. K-L) In March 2025, MRA and MRI were followed up (The left internal carotid artery cavernous segment was unobstructed, and no recurrence of tumor was seen).
The angiography review indicated that the rupture in the cavernous segment of the left internal carotid artery had disappeared, with no contrast agent extravasation (Figure 1H). The stent was well adhered to the vessel wall, and the artery was unobstructed. After routine disinfection and draping, the nasal packing was removed under endoscopy. It was observed that the bleeding in the cavernous segment of the left internal carotid artery had stopped. The external rupture of the left cavernous segment of the internal carotid artery was packed with muscle plasma, and iodoform gauze and expanded sponge were used to pack the nasal cavity. 14 units of red blood cells and 600 ml of plasma were transfused. The specimen was sent for pathological examination. The operation went smoothly. Postoperative blood routine review showed that acute hemorrhagic anemia had been corrected (hemoglobin 119 g/L), and the head CT review showed no intracranial hemorrhage.
Pathological examination suggested schwannoma. One month after the operation, angiography showed that the rupture of the internal carotid artery had completely healed. Follow-up for half a year showed no recurrence of the tumor on MRI (Figures 1I & 1J). In March 2025, the patient was followed up and had no special discomfort complaints. The right eye had no limitation in abduction, and no other abnormal signs were found ((Figures 1K & 1L). The patient is still under follow-up observation.
2. Discussion
Transnasal endoscopic tumor resection is a commonly used surgical approach for schwannoma diseases and is widely applied in clinical practice. However, intracranial arterial injury, as an extremely dangerous complication of such surgeries, remains a potential risk that cannot be ignored during the operation. Specifically, in transnasal endoscopic sphenoid sinus tumor resection, although the rupture of the internal carotid artery has serious consequences, relevant studies indicate that its occurrence rate is relatively low, approximately 0-0.1% [1]. Al Qahtani et al. [2] summarized the common causes of intraoperative rupture of the internal carotid artery, including: anatomically, the thin or absent bone wall between the extradural segment of the internal carotid artery and the sphenoid sinus within the skull increases the risk of injury during surgery; in terms of surgical operation, the surgeon's insufficient familiarity with the local anatomy, rough and excessive traction when separating the tumor from the surrounding tissues, or the use of sharp instruments when approaching the sphenoid sinus and sellar region, may directly puncture the internal carotid artery; in addition, it also includes structural or functional abnormalities of the internal carotid artery wall that cause the artery wall to become thin and lose its normal protection, the internal carotid artery being closely adhered to or even surrounded by the lesion tissue, making separation extremely difficult, and a history of radiotherapy or chemotherapy at the surgical site. Griauzde et al. [3] reported the current status of 4 cases of emergency endovascular treatment for internal carotid artery injury during transsphenoidal surgery: the lesions included 2 cases of macroadenoma of the pituitary gland, 1 case of meningioma and 1 case of chondrosarcoma.
Risk factors for internal carotid artery injury included carotid artery laceration, attachment of the sphenoid septum to the internal carotid artery, and previous radiotherapy for tumors. In 3 patients, the implantation of covered stents achieved hemostasis at the site of internal carotid artery injury. One patient developed delayed bleeding 6 hours after covered stent implantation and underwent successful endovascular occlusion of the internal carotid artery, but died 6 days later. One patient developed internal carotid artery thrombosis during the operation, and thrombectomy, thrombolysis and stent implantation were performed to achieve hemostasis. In 2007, Li MH et al. [4] reported a new product called Willis stent, which was developed for the treatment of internal carotid artery pseudoaneurysms. It can easily reach the target lesion of the internal carotid artery, and the entire stent system is flexible with low resistance when reaching the target lesion, demonstrating good delivery performance and operability. Xu Tianming et al. [5] reported 2 cases of pituitary adenoma and 1 case of optic nerve injury, in which internal carotid artery rupture and bleeding occurred during endoscopic transsphenoidal resection of sellar lesions and optic canal decompression. The Willis covered stent was successfully implanted to repair the rupture, and all 3 patients have recovered well. Fu X et al. [6] reported a case of internal carotid artery rupture during endoscopic transsphenoidal pituitary tumor resection. The Willis covered stent was used for rescue during the operation and successfully sealed the rupture of the internal carotid artery.
The Willis covered stent is made of ultra-thin expanded polytetrafluoroethylene and cobalt-chromium alloy, with a total thickness of only 0.13 mm. It features a sinusoidal open design, which is suitable for tortuous intracranial vessels and closely adheres to the vessel wall. Endovascular isolation can close the fistula, and the operation technique is mature. In this case, the 3.5-16 Willis intracranial covered stent can be directly attached to the fistula with the biological membrane attached to its exterior, precisely blocking the abnormal arterial rupture and restoring the hemodynamics of the lesion area to normal. While occluding the fistula, it ensures the smooth blood flow of the internal carotid artery and venous system. Fu X et al. [6] pointed out that for internal carotid artery injury during endoscopic nasal surgery, covered stent implantation is the best and only method to immediately seal the rupture point and maintain the blood flow of the internal carotid artery.
There were four reasons for the successful rescue of this patient. Firstly, the carotid-cavernous fistula was quickly sealed with iodoform gauze, which stopped the bleeding within minutes. Then, a large amount of blood was transfused in time. Subsequently, digital subtraction angiography was performed promptly. Then, the Willis intracranial covered stent was used to cover the cavernous sinus rupture, successfully sealing the carotid artery rupture. Finally, muscle packing was performed after the stent was placed to ensure complete healing of the rupture. For this case, we have the following experiences: after the rupture of the internal carotid artery, the rupture must be treated urgently, temporarily compressing the bleeding site to avoid acute rapid blood loss of more than 3-4 thousand milliliters; take covered stents or high-flow bypasses to reconstruct the blood flow pathway and avoid ischemic infarction complications in the distal end.
Conflicts of Interest
None.
Author Contributions
Shuai Ma is responsible for collecting various data of patients. During the stage, he has innovated the picture layout in this article. Tie-ZShu Guo and Jian-Hong Li are the chief surgeon and assistant surgeon of this operation. Their efforts have significantly enhanced the quality and comprehensiveness of our study.
REFERENCES
[1] Xiaohai Liu, Ming Feng, Congxin Dai, et
al. “Internal carotid artery injury in the endoscopic transsphenoidal surgery for
pituitary adenoma: an uncommon case and literature review.” Gland Surg, vol.
9, no. 4, pp. 1036-1041, 2020.
View at: Publisher Site
| PubMed
[2] AbdulAziz AlQahtani, Paolo Castelnuovo,
Piero Nicolai, et al. “Injury of the internal carotid artery during endoscopic skull
base surgery: prevention and management protocol.” Otolaryngol Clin North Am,
vol. 49, no. 1, pp. 237-252, 2016. View at: Publisher Site | PubMed
[3] Julius Griauzde, Joseph J Gemmete, Aditya
S Pandey, et al. “Emergency reconstructive endovascular management of intraoperative
complications involving the internal carotid artery from trans-sphenoidal surgery.”
J Neurointerv Surg, vol.7, no. 1, pp.67-71, 2015. View at: Publisher Site | PubMed
[4] M-H Li, Y-D Li, B-L Gao, et al. “A new
covered stent designed for intracranial vasculature: application in the management
of pseudoaneurysms of the cranial internal carotid artery.” AJNR Am J Neuroradiol,
vol. 28, no. 8, pp. 1579-1585, 2007. View at: Publisher
Site | PubMed
[5] XU TM, CAI DY, XU GQ, et al. “Emergency
reconstruction of iatrogenic internal carotid rupture with Willis covered stent
implantation: preliminary experience in 3 cases.” Journal of Interventional Radiology,
vol. 30, no. 6, pp. 608-611, 2021.
[6] Xiaojie Fu, Tao Quan, Yongjie Yuan, et al. “Devastating iatrogenic internal carotid artery rupture in endoscopic endonasal surgery rescued by a covered stent.” Clin Case Rep, vol. 9, no. 8, pp. e04277, 2021. View at: Publisher Site | PubMed
