Received: Sun 20, Aug 2023
Accepted: Wed 06, Sep 2023
Abstract
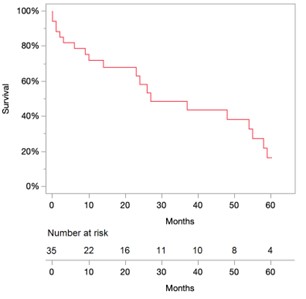
Objective: To analyze five-year clinical and echocardiographic outcomes in patients presenting with acute cardiogenic shock (CS) who underwent transcatheter edge-to-edge repair (TEER) for moderate or severe mitral valve regurgitation (MR). Methods: All consecutive patients who underwent TEER for MR were identified from our institutional medical records between 2015 and 2022. Patients presenting with CS undergoing TEER were included in the primary analysis. MR was diagnosed based on patient's echocardiographic findings and CS was diagnosed according to the definition in the TVT registry and/or presence of inotrope use prior to procedure and/or mechanical circulatory support prior to procedure. Kaplan-Meier survival curves were constructed to analyze outcomes. Primary outcome was five-year incidence of all-cause death. Secondary outcomes were major adverse cardiovascular and cerebrovascular events (MACCE) and readmission for heart failure (HF). Results: A total of 35 patients were included in the study. Mean age was 81±10.4 years and 16 patients (45.7%) were male. Mean STS-score was 10.2±7.1. Nine (25.7%) patients had prior myocardial infarction (MI), 22 (62.8%) had previous atrial fibrillation, while 9 (25.7%) patients were hospitalized for HF within the past year. MR etiology was degenerative (71.4%), functional (22.9%), and mixed (5.7%). Prior to presentation with CS, NYHA classification included 2 (5,7%) patients in class I, 6 (17.1%) in class II, 13 (37.1%) in class III, and 14 (40%) in class IV. Pre-procedural mean LVEF was 56.4 ± 13%. Procedural characteristics included mean procedural time (from access to guide removal) of 2.0 ± 0.6 hours, > 1 implanted device in 14 (40.0%) patients, 1 patient had a single leaflet attachment. There was no procedural device embolism, device thrombosis, conversion to sternotomy, life threatening bleeding, stroke, MI, or death. Mean postoperative length of stay was 5.1 ± 4.4 days. During their hospital stay, a transient ischemic attack event occurred in 1 patient; however, no MI, stroke, or death were observed in any patient. During the follow-up, 13 (37.1%) patients were readmitted for HF, 1 patient needed mitral valve replacement and 1 patient needed new TEER. At 5 years, only 4 (11.4%) patients were alive. Conclusion: Despite excellent procedural and early outcomes for patients with significant MR and CS undergoing TEER, poor survival was observed after 5 years, which may be related to advanced age of this cohort.
Keywords
TEER, cardiogenic shock, MitraClip, mitral regurgitation
1. Central Message
Patients with significant MR and CS undergoing TEER have excellent procedural and early outcomes. However, long-term mortality remains high. Long-term Survival after TEER in patients with mitral valve regurgitation and cardiogenic shock.
2. Introduction
Cardiogenic shock is associated with high mortality and has limited treatment options including inotropes, vasopressors, and mechanical support. Furthermore, concomitant valvopathies are commonly present in CS patients and multiple studies have evidenced that valvular heart disease increases the risk of mortality in patients presenting with CS [1]. In addition, the presence of myocardial infarction (MI) and mitral regurgitation (MR) is associated with an increased risk of mortality [2-4]. Although surgical treatment is the first-line treatment for severe MR, TEER emerged as a promising treatment for patients at high surgical risk [5, 6]. The short-term clinical outcomes and feasibility of TEER have been investigated in patients with CS with positive results [6-8]. However, the long-term outcomes of TEER in the context of CS remain unclear and warrant investigation. Herein, we investigated 5-year outcomes of patients with moderate or greater MR and CS undergoing TEER in our institution.
3. Methods
3.1. Study Cohort
The STS/ACC TVT database was searched to identify all consecutive patients older than 18 years old who presented with CS and underwent TEER with the MitraClip device (Abbott Vascular) from June 2015 to October 2022 at Lankenau Heart Institute. Thirty-five patients were identified in the primary search. MR was diagnosed based on the patient’s preoperative transthoracic (TTE) and transesophageal echocardiography (TEE) findings, and CS was diagnosed based on STS/ACC TVT registry definition. TVT registry defined CS based on the following criteria: sustained (>30 min) episode of systolic blood pressure <90 mm Hg and/or cardiac index <2.2 L/in per square meter determined to be secondary to cardiac dysfunction and/or the requirement for parenteral inotropic or vasopressor agents or mechanical support (eg, IABP, extracorporeal circulation, VADs) to maintain blood pressure and cardiac index above those specified levels [9]. Patients presenting with CS were medically optimized and within 1-2 days were treated with TEER. HF readmission was defined as: hospitalization >=24 hours (including emergency room stay), clinical signs and/or symptoms of heart failure (including, but not limited to, new or worsening dyspnea, orthopnea, paroxysmal nocturnal dyspnea, increasing fatigue, worsening functional capacity or activity intolerance, or signs and/or symptoms of volume overload.), and intravenous (e.g, diuretic or vasoactive therapy) or invasive (e.g., ultrafiltration, IABP, mechanical assistance) treatment for heart failure [10]. This study was approved by the local institutional review board.
3.2. Clinical Outcomes
Baseline echocardiographic findings included left ventricular ejection fraction (EF), left ventricular internal diastolic dimension (LVIDd), moderate/ or severe aortic regurgitation, aortic stenosis left ventricular internal systolic dimension (LVIDs), MR severity, and MR etiology (functional, degenerative, mixed, other), and were retrospectively collected. MR severity was categorized as 1+ (none/trivial/mild), 2+ (moderate), 3+ (moderate-severe), and 4+ (severe) according to American Society of Echocardiography recommendations. Device success was determined based on the reduction of MR by ≥1+ and absolute MR grade to a final level of MR ≤ 2+ in addition to freedom from conversion to open cardiac surgery. Primary outcome was five-year incidence of all-cause death. Secondary outcomes were major adverse cardiovascular and cerebrovascular events (MACCE) and readmission for heart failure (HF) during 5-year follow-up.
3.3. Statistical Analysis
Continuous variables were reported as mean ± standard deviation (SD) or median (25th and 75th percentiles), and categorical variables were summarized as counts and percentages. 5-year mortality and HF readmission status were available for all patients. Kaplan-Meier survival curve was constructed to evaluate survival using JMP 13.1 software (SAS).
4. Results
A total of 35 patients were identified through the STS/ACC TVT registry. CS was determined according to presence of coding for CS, or/and mechanical circulatory support, and/or inotrope use. Mean age was 81±10.4 years, 16 patients (45.7%) were male, and 30 patients (85.7%) were of white race (Table 1). Mean STS-score was 10.2±7.1. Three (8.6%) patients had a prior cerebrovascular event, 9 (25.7%) had prior myocardial infarction, 22 (62.8%) had previous atrial fibrillation, while 9 (25.7%) patients were hospitalized for heart failure within the past year. MR etiology was degenerative (74.3%), functional (20.0%), and mixed (5.7%). NYHA classification included 2 (5,7%) patients in class I, 6 (17.1%) in class II, 13 (37.1%) in class III, and 14 (40%) in class IV. Pre-operative mean left ventricular ejection fraction was 56.4 ± 13%. Procedural characteristics included mean operative time of 2.0 ± 0.6 hours, > 1 implanted device in 14 (40.0%) patients, and one patient had a single leaflet attachment. Device success was reached in 60% of cases. No device embolization, device thrombosis, conversion to sternotomy, life-threatening bleeding, stroke, myocardial infarction, or death was observed (Table 3). Mean hospital length of stay was 9.3 ± 6.6 days. Seven (20.0%) patients were discharged to the transitional care unit, 3 (8.5%) to the skilled nursing facility, and 25 (71.4%) to home. During the hospital stay, transient ischemic attack event occurred in only one patient; however, no myocardial infarction, stroke, or death were observed in any patient. The mortality rate at 30 days was 8.6%. At 5 years, only four (11.4%) patients were alive (Figure 1). Cardiac mortality occurred in 25 (80.6%) patients, 2 (6.4%) patients had fatal stroke and 4 (13%) patients died due to other causes. Follow-up echocardiographic outcomes are described in (Table 4).
TABLE 1: Baseline
characteristics.
|
|
All patients (N=35) |
|
Age (years) |
81 +/- 10.4 |
|
Male |
16 (45.7%) |
|
Race |
|
|
White |
30 (85.7%) |
|
Black |
5 (14.3%) |
|
Asian |
0 (0.0%) |
|
Hispanic/Latino |
0 (0.0%) |
|
BMI (kg/sqm) |
24.64 +/- 4.8 |
|
Hypertension |
33 (94.2%) |
|
Diabetes |
10 (28.5%) |
|
Current Smoker |
1 (2.8%) |
|
Chronic Lung Disease |
8 (22.8%) |
|
Home Oxygen Use |
2 (5.7%) |
|
Endocarditis |
1 (2.8%) |
|
Prior Myocardial Infarction |
9 (25.7%) |
|
Prior Percutaneous Coronary Intervention |
14 (40%) |
|
Atrial Fibrillation/Flutter |
22 (62.8%) |
|
Peripheral Vascular Disease |
6 (17.1%) |
|
Any Prior Stroke |
2 (5.7%) |
|
Transient Ischemic Attack |
1 (2.8%) |
|
Pacemaker |
11 (31.4%) |
|
Creatinine (mg/dL) Mean B.P mmHg |
1.5 +/- 0.9 76/34 mmHg |
|
CAD - No. of disease vessels |
|
|
None |
22 (62.8%) |
|
One |
5 (14.2%) |
|
Two |
3 (8.5%) |
|
Three |
5 (14.2%) |
|
Left Main Stenosis ≥ 50% |
0 (0.0%) |
|
Acute coronary syndrome |
8 (22.8%) |
|
NYHA Class (in preceding 2 wks) |
|
|
I |
2 (5.7%) |
|
II |
6 (17.1%) |
|
III |
13 (37.1%) |
|
IV |
14 (40%) |
|
Pre-procedural IABP use |
14 (40%) |
|
Cardiac arrest (within 24 hrs) |
0 (0.0%) |
|
HF Hospitalization within past year |
9 (25.7%) |
|
STS 2007 Operative Risk Score (%) - Mean/SD |
10.2 +/- 7.1 |
|
STS 2007 Operative Risk Score (%) -
Median/25-75th |
8.27 (5.35, 12.6) |
Number (%), mean +/-
standard deviation (SD), median (25th, 75th).
TABLE 2: Baseline
investigations.
|
|
All patients |
|
(N=35) |
|
|
Echocardiography |
|
|
LVEF (%) - mean±SD |
56.4 +/- 13 |
|
LVEF (%) - median (25th, 75th) |
60 (46.1, 65.0) |
|
Left Ventricular Internal Systolic Dimension (cm)
- mean ± SD |
4.2 +/- 2.3 |
|
Left Ventricular Internal Systolic Dimension (cm)
- median (25th,75th) |
3.98 (2.7, 5.1) |
|
Left Ventricular Internal Diastolic Dimension
(cm) - mean ± SD |
5.6 +/- 2.1 |
|
Left Ventricular Internal Diastolic Dimension
(cm) - median (25th,75th) |
5.4 (4.2, 6.0) |
|
Aortic regurgitation (≥ moderate) |
2 (5.7%) |
|
Aortic stenosis |
3 (8.5%) |
|
Mitral Regurgitation - Severity |
|
|
Mild |
0 (0.0%) |
|
Moderate |
3 (8.5%) |
|
Moderate/Severe |
3 (8.5%) |
|
Severe |
29 (82.8) |
|
Mitral regurgitation - Etiology* |
|
|
Functional |
7 (20.0%) |
|
Degenerative |
26 (74.3%) |
|
Mixed |
2 (5.7%) |
|
Other |
0 (0.0%) |
Number (%), mean +/-
standard deviation (SD), median (25th, 75th). *This
section presents proportions relative to the total number of patients with each
specific MR etiology.
TABLE 3: Procedural
and in-hospital characteristics.
|
|
All Patients (N=35) |
|
Procedural Characteristics |
|
|
Admission to device implant (days) |
|
|
Mean +/- S.D. |
4.2 +/- 3.7 |
|
Median (25th, 75th) |
5 (0.0, 7.0) |
|
Procedural duration (hours) |
|
|
Mean +/- S.D. |
2.0 +/- 0.6 |
|
Median (25th, 75th) |
1.8 (1.6, 2.2) |
|
Number of devices implanted |
|
|
1 device |
21 (60.0%) |
|
>1 devices |
14 (40.0%) |
|
Site of device implant |
|
|
A2-P2 |
33 (94.2%) |
|
Device failure |
14 (40.0%) |
|
Transseptal Complication |
0 (0.0%) |
|
Single leaflet device attachment |
1 (2.8%) |
|
Device embolism |
0 (0.0%) |
|
Device thrombosis |
0 (0.0%) |
|
Other |
0 (0.0%) |
|
Converted to open heart surgery |
0 (0.0%) |
|
In-Hospital Course |
|
|
Bleeding |
|
|
VARC Major bleeding/not life
threatening/disabling |
0 (0.0%) |
|
VARC life threatening/disabling |
0 (0.0%) |
|
Access site hematoma |
|
|
MI |
0 (0.0%) |
|
Stroke |
0 (0.0%) |
|
Transient ischemic attack |
1 (2.8%) |
|
Overall length of stay (days) |
|
|
Mean +/- S.D. |
9.3 +/- 6.6 |
|
Median (25th, 75th) |
10 (1.5, 12.5) |
|
Discharge location |
|
|
Home |
25 (71.4%) |
|
Extended Care/TCU/Rehab |
7 (20.0%) |
|
Other Acute Care Hospital |
0 (0.0%) |
|
Skilled Nursing Facility |
3 (8.5%) |
|
Hospice Care |
0 (0.0%) |
|
Left Against Medical Advice |
0 (0.0%) |
|
Other |
0 (0.0%) |
Number (%), mean +/-
standard deviation (SD), median (25th, 75th).
TABLE 4: Echocardiographic
outcomes at follow-up.
|
Follow-up Outcomes |
N=35 |
|
EF
(mean/SD) % |
56.2
(12.4) |
|
MR
Grade |
|
|
None n
(%) |
27
(77.1%) |
|
Mild n
(%) |
6
(17.1%) |
|
Moderate
n (%) |
2
(5.7%) |
|
Severe
n (%) |
0 (0%) |
|
Stroke
Volume ml (mean/SD) |
65.6
(30.3) |
|
LVEDD
cm (mean/SD) |
7.1
(10.9) |
|
LVESD
cm (mean/SD) |
4.3
(3.6) |
|
LVEDV
ml (mean/SD) |
96.3
(48.8) |
|
LVESV
ml (mean/SD) |
44.6
(33.6) |
|
Mean
Gradient (mmHg) |
4 (3-6) |
|
LAESV
ml (mean/SD) |
92.2
(39.2) |
|
RVSP mmHg
(mean/SD) |
43.1
(13.7) |
MR: mitral regurgitation;
LVEDD: left ventricular end diastolic diameter; LVESD: left ventricular
end-systolic diameter; LVEDV: left ventricular end diastolic volume; LVESV:
left ventricular end-systolic volume; LAESV: left atrial systolic volume; RVSP:
right ventricular systolic pressure.
5. Discussion
To the best of our knowledge, this is the first study with 5-year outcomes follow-up of patients undergoing TEER in the setting of CS and MR. In our institutional experience, we observed that this population is of advanced age (over 80 years) and high surgical risk (mean STS score over 10%) with advanced heart failure with high NYHA III/IV (over three-quarters of the population). Previous studies showed that successful reduction in MR is associated with better 1-year survival and lower hospitalization because of HF [2, 8]. In our study, we achieved 60% of device success and 1 year mortality rate was roughly 30%.
Simard et al. [2] investigated the characteristics and outcomes of consecutive patients with significant mitral regurgitation (MR) and CS who underwent TEER using the STS/ACC TVT registry. The authors found that successful MR reduction is achievable in most patients with CS and is associated with significantly lower mortality and HF hospitalization at 1 year. However, the authors reported a device success rate of 85.6% (which was higher than our success rate of 60%). Survival remains poor after 5 years despite the procedure, but we should keep in mind that this might be related to the high-risk profile of this population and its short life expectancy due to advanced age.
One aspect which remains unclear is the fact that the patients in our study presented with CS as the primary reason and were found to have MR, but whether the CS was caused by MR is hard to establish because we do not have previous echocardiograms showing the presence/absence of MR for most of the patients to establish a timeline. Although we observed a poor survival at 5 years, we do not know the expected survival in this population. We considered using the COAPT risk score [11] to predict survival in this population. However, it would have been inappropriate to apply this score because this population is a mix of functional and degenerative MR, while the score was exclusively created for functional MR.
The capital minos study [12] is an ongoing trial aiming to determine whether TEER improves outcomes in patients with CS and MR in comparison with medical therapy alone and will be an important step in optimizing treatment for this high-risk patient population.
6. Conclusion
Patients with significant mitral regurgitation and cardiogenic shock undergoing transcatheter edge-to-edge repair had excellent immediate postoperative survival considering the scenario. However, device failure and 5-year mortality remain high.
Limitations
Although this study does not have a comparison of TEER vs no-TEER, it can help establish the potential 5-year efficacy of this procedure by documenting clinical and echocardiographic outcomes in this patient cohort. Additional limitations include the small number of included patients (n=35), the presence of degenerative MR in 2/3 of the cases, lack of a control group, and lack of granularity on inotropes number. While it is intuitive that patients presenting with CS have hypotension, the definition of CS according to TVT does not include hypotension among the definitions criteria.
Conflicts of Interest
None.
Funding
None.
REFERENCES
[1] Nino Mihatov, Ramya C Mosarla, Ajay J
Kirtane, et al. “Outcomes Associated With Peripheral Artery Disease in
Myocardial Infarction With Cardiogenic Shock.” J Am Coll Cardiol, vol.
79, no. 13, pp. 1223-1235, 2022. View at: Publisher Site | PubMed
[2] Trevor Simard, Sreek Vemulapalli,
Richard G Jung, et al. “Transcatheter Edge-to-Edge Mitral Valve Repair in
Patients With Severe Mitral Regurgitation and Cardiogenic Shock.” J Am Coll
Cardiol, vol. 80, no. 22, pp. 2072-2084, 2022. View at: Publisher Site | PubMed
[3] C R Thompson, C E Buller, L A
Sleeper, et al. “Cardiogenic shock due to acute severe mitral regurgitation
complicating acute myocardial infarction: a report from the SHOCK Trial
Registry. SHould we use emergently revascularize Occluded Coronaries in
cardiogenic shocK?” J Am Coll Cardiol, vol. 36, no. 3 Suppl A, pp.
1104-1109, 2000. View at: Publisher Site | PubMed
[4] Holger Thiele, E. Magnus Ohman,
Steffen Desch, et al. “Management of cardiogenic shock.” European Heart
Journal, vol. 36, no. 20, pp. 1223-1230, 2015. View at: Publisher Site
[5] Michael Mack, John D Carroll, Vinod
Thourani, et al. “Transcatheter Mitral Valve Therapy in the United States: A
Report from the STS/ACC TVT Registry.” Ann Thorac Surg, vol. 113, no. 1,
pp. 337-365, 2022. View at: Publisher Site | PubMed
[6] Santiago Garcia, Said Alsidawi,
Richard Bae, et al. “Percutaneous Mitral Valve Repair With MitraClip in
Inoperable Patients With Severe Mitral Regurgitation Complicated by Cardiogenic
Shock.” J Invasive Cardiol, vol. 32, no. 6, pp. 228-231, 2020. View at: PubMed
[7] Nimrod Perel, Elad Asher, Luoay Taha,
et al. “Urgent Transcatheter Edge-to-Edge Repair for Severe Mitral
Regurgitation in Patients with Refractory Cardiogenic Shock.” J Clin Med,
vol. 11, no. 19, pp. 5617, 2022. View at: Publisher Site | PubMed
[8] Chak-Yu So, Guson Kang, James C Lee,
et al. “Transcatheter Edge-to-Edge Repair for Acute Mitral Regurgitation With
Cardiogenic Shock Secondary to Mechanical Complication.” Cardiovasc Revasc
Med, vol. 45, pp. 44-50, 2022. View at: Publisher Site | PubMed
[9] Christopher P Cannon, Ralph G
Brindis, Bernard R Chaitman, et al. “2013 ACCF/AHA Key Data Elements and
Definitions for Measuring the Clinical Management and Outcomes of Patients With
Acute Coronary Syndromes and Coronary Artery Disease: A Report of the American
College of Cardiology Foundation/American Heart Association Task Force on
Clinical Data Standards (Writing Committee to Develop Acute Coronary Syndromes
and Coronary Artery Disease Clinical Data Standards).” Circulation, vol.
127, no. 9, pp. 1052-1089, 2013. View at: Publisher Site | PubMed
[10]
STS/ACC
TVT registry data dictionary [Internet].
[11] Neeraj Shah, Mahesh V Madhavan, William A Gray, et al. “Prediction of Death or HF Hospitalization in Patients With Severe FMR.” JACC: Cardiovascular Interventions, vol. 15, no. 19, pp. 1893-1905, 2022. View at: Publisher Site | PubMed
[12] Simon Parlow, Pietro Di Santo, Richard G Jung, et al. “Transcatheter mitral valve repair for inotrope dependent cardiogenic shock - Design and rationale of the CAPITAL MINOS trial.” Am Heart J, vol. 254, pp. 81-87, 2022. View at: Publisher Site | PubMed
