Received: Thu 11, Jul 2024
Accepted: Sat 31, Aug 2024
Abstract
Purpose: This study aimed to assess the impact of MAKO robot-assisted total knee arthroplasty on restoring patients' physiological trochlear groove and evaluating its influence on joint function.
Method: This study included patients who underwent primary unilateral total knee arthroplasty using MAKO robot. Patients were randomly assigned to the trochlear groove reconstruction group (TG reconstruction group) (n=95) and the control group (n=96). In the TG reconstruction group, the rotational angle of the femoral component was adjusted to restore the patient's original trochlear groove morphology, while the control group received conventional preoperative planning (TEA=0°). Outcome measures included patellofemoral index, patellar tilt angle, advanced activities, knee range of motion (ROM), knee society score (KSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the medical outcomes study 36-item short-form health survey (SF-36), five times sit-to-stand test (5xSST), and occurrence of adverse events. Follow-up assessments were conducted at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively.
Result: There were significant statistical differences in preoperative TEA planning between the two groups (1.42±1.89 vs 0° p=0.00). Postoperatively, the TG reconstruction group showed better patellofemoral index (1.28±0.58 vs 1.72±0.78, p=0.040) and patellar tilt angle (2.82±2.32 vs 9.40±7.30, p=0.040) compared to the control group. At 1 year postoperatively, the TG reconstruction group exhibited superior KSS (86.03±10.35 vs 81.09±10.74, p=0.006) and WOMAC (6.50±6.64 vs 10.52±10.23, p=0.014) compared to the control group. Additionally, at 1 year postoperatively, the TG reconstruction group performed better than the control group in terms of knee ROM (126.43±9.94 vs 120.75±11.63 p=0.006), 5xSST (14.24±4.78 vs 16.88±5.88 p=0.026), carrying a shopping bag for a block (75% vs 57% p=0.032), and squatting (42% vs 22% p=0.002). There was no significant difference between the two groups in terms of SF-36 scores. There were no significant differences in the occurrence of adverse events between the two groups.
Conclusion: MAKO robot-assisted total knee arthroplasty, which adjusts the rotational alignment of the femoral component to restore the patient's physiological trochlear groove morphology, can enhance joint function in patients. This underscores the importance of personalized preoperative planning in MAKO robot-assisted total knee arthroplasty.
Keywords
MAKO robot-assisted total knee arthroplasty, femoral component rotation, patellofemoral groove alignment, advanced activities
1. Introduction
Research indicates that the complication rate of total knee arthroplasty (TKA) can be as high as 12% [1-4]. This includes chronic pain, prosthesis wear, malalignment, and patellar tracking abnormalities [1, 4-8]. Among these, patellofemoral complications are a major reason for revision surgery. Most patellofemoral complications are reported to be related to abnormal patellar tracking [9]. Changes in patellar tracking may lead to increased polyethylene wear, aseptic loosening, and patellar instability. Literature suggests that femoral component malposition is a significant cause of abnormal patellar tracking [10-12]. This is because improper rotation of the femoral component can result in patellar maltracking, leading to abnormal stress on the patella [13-16]. This can significantly impact the functionality of the patient's knee joint function and even lead to revision surgery.
Currently, the typical placement of the femoral component in total knee arthroplasty (TKA) uses the transepicondylar axis as the rotational axis of the knee joint. However, determining the knee joint rotational axis during surgery remains challenging [17]. Auxiliary methods such as whiteside's line and posterior condylar axis also have inherent errors in determining the knee joint rotational axis [18, 19]. Additionally, there are also some controversies in the placement of the femoral component: Fuchs [20] and Woiczinski et al. [16] suggested placing the femoral component in the medial or externally rotated position. Steinbrück et al. [10], suggested placing the femoral component 3°-6° externally rotated relative to the transepicondylar axis (TEA) while maintaining soft tissue balance. Due to individual anatomical variations, personalized surgical planning may offer a better solution [21, 22].
In recent years, the introduction of robotic-assisted surgery has provided new prospects for total knee arthroplasty. Particularly in surgical planning and precision, robotic-assisted TKA has shown significant advantages [23, 24]. Through robotic assistance, precise preoperative planning can be implemented, and adjustments to the rotational angle of the prosthesis can be made accurately.
Therefore, this study aims to adjust the rotation angle of the femoral component, determine the rotational axis of the knee joint, restore the patient's physiological trochlear groove morphology, and adapt to the patellar morphology. Additionally, it aims to evaluate the impact of these adjustments on knee joint function, aiming to provide more precise guidance and references for total knee arthroplasty.
2. Methods
2.1. Data Collection
This study was approved by the Ethics Review Committee of the Chinese People's Liberation Army Medical College, with the approval number of S2021-094-01. Patients undergoing MAKO robot-assisted total knee arthroplasty at the First Medical Center of the Chinese PLA General Hospital from January 2022 to March 2023 were consecutively enrolled. Inclusion criteria were as follows: patients aged 18 years or older undergoing primary unilateral total knee arthroplasty due to osteoarthritis. Exclusion criteria included: i) history of knee surgery or traumatic osteoarthritis within the past 3 months. ii) Patients unwilling to participate in the study. iii) Patients planning or having undergone contralateral knee surgery within 90 days. iv) Patients with severe patellofemoral arthritis (Grades III-IV). v) Patients with trochlea dysplasia.
Baseline data collected included: age, gender, BMI, comorbidities, surgery time, knee range of motion (ROM), knee society score (KSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), The medical outcomes study 36-item short-form health survey (SF-36) and five times sit-to-stand test (5xSST). Postoperatively, patellofemoral index and patellar tilt angles were measured. Follow up with patients at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively. Follow-up assessments included: WOMAC, KSS, SF-36, knee joint ROM, and 5xSST. Functional outcomes related to squatting and advanced activities at 1 year postoperatively were evaluated using specific questions from the KSS score. Patients scoring 4 or 5 points were defined as capable of squatting, while those scoring below 4 points were defined as unable to squat. Similar analytical methods were applied to other questions. Postoperative complications and adverse events were recorded during follow-up.
2.2. Surgical Technique
Patients were randomly assigned to either the control or trochlear groove reconstruction group (TG reconstruction group). All patients underwent a medial parapatellar approach. The Mako TKA system (Stryker, Mahwah, NJ) was used in this study. This is a CT-based tactile platform that assists surgeons in precise bone resection and provides real-time feedback during ligament balancing [25]. Preoperatively, CT scans were performed to create a 3D model of the knee joint based on which surgical planning was conducted by surgeons.
2.3. Trochlear Groove Reconstruction Group (TG Reconstruction Group)
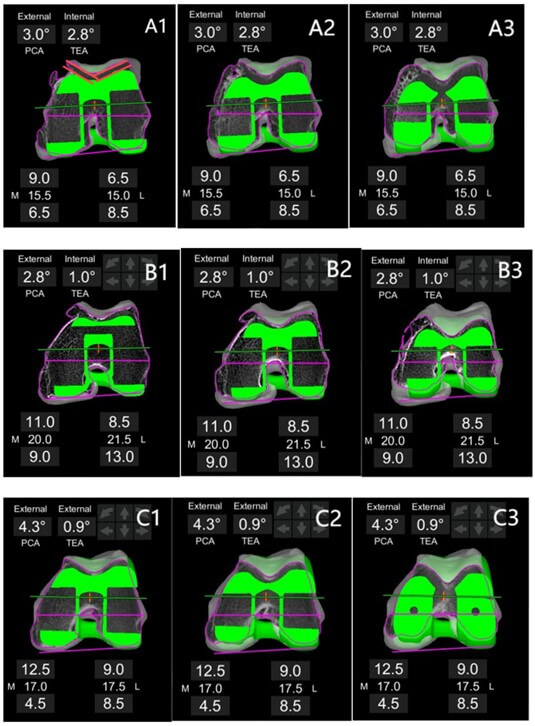
Patients in the TG reconstruction group underwent preoperative planning using the Mako surgical system. Preoperative planning was standardized and performed by one physician (ZGQ). During preoperative planning, adjustments were made to the rotation angle of the femoral component to ensure as close a restoration of the native trochlear morphology as possible on axial plane sections: specifically, to align the femoral component's trochlear groove “parallel” to the patient's native groove, aiming for optimal patellofemoral alignment. “parallel” was defined as an angle difference of less than 3 degrees between the trochlear groove of the knee prosthesis and the native knee, with equal medial and lateral spacing wherever feasible (Figure 1).
2.4. Control Group
The control group followed an initial plan with a femoral component TEA angle of 0° and employed a standardized bone resection method during preoperative planning. All patients were assessed during follow-up evaluations by the same physician who was blinded to the group assignments. Both groups of patients underwent postoperative rehabilitation using a home-based recovery manual. Outpatient follow-up and guidance were conducted at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively. Based on our preliminary results, the squatting rate was 35% in the experimental group compared to 17% in the control group [26]. Therefore, each group requires 90 patients to meet statistical requirements.
2.5. Statistical Methods
Data normality was assessed using the Shapiro-Wilk test. Variables that met the criteria for normal distribution (e.g., KSS, WOMAC, SF-36 scores) are presented as mean ± standard deviation (SD) and were compared using independent t-tests. Non-normally distributed variables are presented as median with interquartile range, and group comparisons were made using the chi-square test. A significant level of P ≤ 0.05 was considered statistically significant. Patients with missing data at two or more follow-up visits were considered invalid and were excluded from the study. All data were analyzed using SPSS version 26.0 (IBM, Armonk, NY, USA).
3. Results
A total of 244 patients who underwent MAKO total knee arthroplasty at the First Medical Center of the PLA General Hospital from January 2022 to March 2023 were included in the study. 24 patients were excluded due to severe patellofemoral arthritis, 5 patients were excluded due to traumatic osteoarthritis, and 20 patients were excluded due to patellar dysplasia. There were 97 patients in the TG reconstruction group and 98 patients in the control group. One patient in the TG reconstruction group withdrew from the study due to early postoperative periprosthetic joint infection. One patient from the TG reconstruction group and two patients from the control group were lost to follow-up. A total of 95 patients in the TG reconstruction group and 96 patients in the control group were included in the analysis (Figure 2). There were no significant differences between the two groups in terms of age, gender, surgical time, preoperative KSS, WOMAC, SF-36, and time for 5xSST. There were no statistically significant differences between the two groups in terms of femoral component flexion and tibial component slope (Table 1).
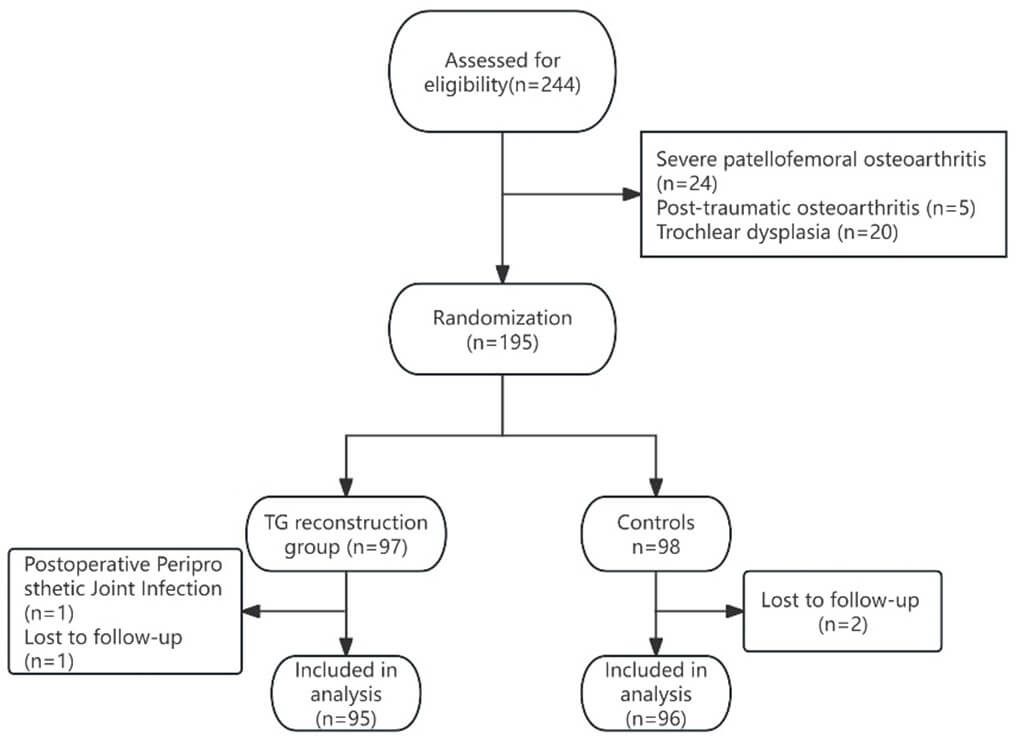
Table 1.
Comparison of preoperative baseline characteristics between the TG
reconstruction group and the control group.
|
|
TG reconstruction group |
P Value |
|
|
Mean age |
65.30±6.37 |
66.02±8.76 |
0.572 |
|
BMI |
26.94±2.72 |
26.83±3.10 |
0.821 |
|
Surgical duration |
68.37±19.36 |
66.51±19.00 |
0.665 |
|
Proportion of women |
77% |
82% |
0.166 |
|
Comorbidities |
|
|
|
|
COPD |
5% |
6% |
0.770 |
|
Coronary heart disease |
32% |
35% |
0.688 |
|
Diabetes |
25% |
27% |
0.813 |
|
Hypertension |
37% |
44% |
0.368 |
|
Other |
12% |
14% |
0.632 |
|
TEA |
1.42±1.89 |
0±0 |
0.000 |
|
PCA |
3.95±1.76 |
2.32±2.03 |
0.000 |
|
Femoral prosthesis(flexion) |
3.26±1.74 |
3.22±1.82 |
0.895 |
|
Tibial prosthesis (slope) |
2.61±1.34 |
2.52±1.59 |
0.650 |
|
Range of motion (flexion) |
108.59±18.20 |
105.12±13.97 |
0.226 |
|
KSS |
41.78±15.11 |
39.73±13.58 |
0.244 |
|
5xSST |
20.28±10.36 |
18.38±15.46 |
0.569 |
|
WOMAC |
|
|
|
|
42.39±11.87 |
45.87±11.83 |
0.243 |
|
|
Pain |
9.94±3.07 |
10.89±2.72 |
0.248 |
|
Stiffness |
2.89±2.47 |
3.29±1.69 |
0.480 |
|
Physical
function |
29.54±8.74 |
30.89±10.02 |
0.530 |
|
SF-36 |
|
|
|
|
Physical functioning |
35.33±13.94 |
28.97±15.52 |
0.172 |
|
Role-physical |
18.33±20.84 |
24.36±42.33 |
0.341 |
|
Bodily pain |
30.67±10.56 |
36.59±14.77 |
0.163 |
|
General health |
56.00±18.57 |
61.95±22.15 |
0.319 |
|
Vitality |
61.00±17.94 |
60.00±26.38 |
0.893 |
|
Social functioning |
45.00±20.48 |
54.48±18.69 |
0.110 |
|
Role-emotional |
27.76±37.76 |
29.88±40.99 |
0.297 |
|
Mental health |
77.6±22.81 |
73.85±27.60 |
0.628 |
|
Health transition |
63.33±20.91 |
63.46±24.89 |
0.985 |
TG reconstruction group:
Trochlear groove reconstruction group; BMI: Body Mass Index; COPD: Chronic
Obstructive Pulmonary Disease; WOMAC: The Western Ontario and Mcmaster
Universities Osteoarthritis Index; KSS: Keen Society Score;
SF-36: The Short Form-36 Questionnaire; 5xSST: Five Times
Sit-to-Stand Test.
In the TG reconstruction group, the mean external rotation of the femoral component relative to the TEA was 1.42°±1.89°, compared to 0° in the control group. The mean external rotation of the PCA in the TG reconstruction group was 3.95° ± 1.76°, while in the control group it was 2.32° ± 2.03°. There were statistically significant differences between the two groups (p=0.000 for both comparisons) (Figures 3 & 4). The TG reconstruction group had a better patellofemoral index (1.28±0.58 vs 1.72±0.78, p=0.040) and patellar inclination angle (2.82°±2.32° vs 9.40°±7.30°) compared to the control group (Figure 5). At 1 year postoperatively, the squatting rate was 43% in the TG reconstruction group and 22% in the control group, with a statistically significant difference (p=0.002); The TG reconstruction group also performed better in “Carrying a shopping bag for a block” (75% vs 57%, p=0.032). “Climbing a ladder or step stool” showed nearly statistically significant differences between the TG reconstruction and control groups (41% vs 32%, p=0.067). At 1 year postoperatively, the TG reconstruction group showed better knee ROM (126.43° ± 9.94° vs 120.75° ± 11.63°, p=0.006) and time to 5xSST (14.24 ± 4.78 vs 16.88 ± 5.88 seconds, p=0.026) compared to the control group (Table 2) (Figures 6 & 7).
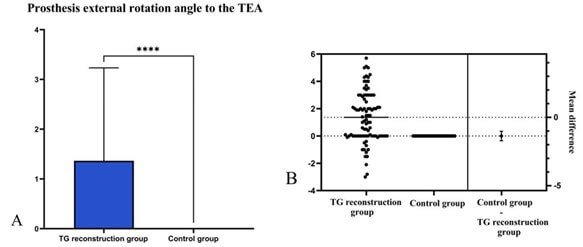
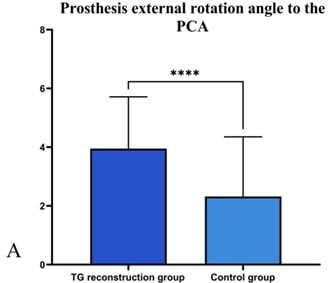
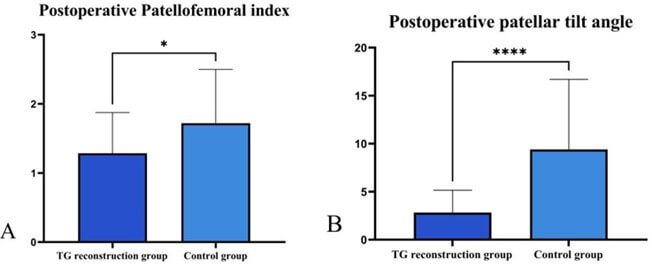

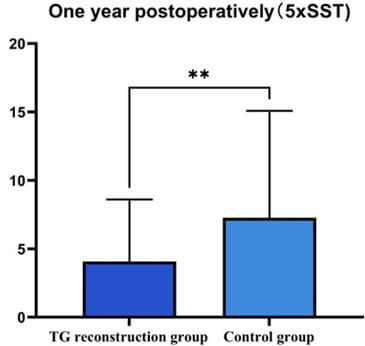
Table 2.
Comparison of preoperative and postoperative HKA (hip-knee-ankle) angle,
patellofemoral index, and patellar tilt angle between the Trochlear groove
reconstruction group and the control group. Comparison of knee joint range of
motion, 5xSST, and advanced activities between the two groups at 1 year
postoperatively. 5xSST: Five Times Sit-to-Stand Test.
|
|
TG reconstruction group |
Control group |
P Value |
|
Preoperative |
|
|
|
|
HKA |
171.4±6.17 |
170.40±6.38 |
0.762 |
|
Patellofemoral index |
1.54±0.86 |
1.60±0.82 |
0.762 |
|
Patellar
tilt angle |
9.28±6.34 |
10.53±6.72 |
0.38 |
|
Postoperative |
|
|
|
|
HKA |
177.92±1.72 |
177.38±2.25 |
0.895 |
|
Patellofemoral index |
1.28±0.58 |
1.72±0.78 |
0.040 |
|
Patellar
tilt angle |
2.82±2.32 |
9.40±7.30 |
0.000 |
|
Range of motion |
126.43±9.94 |
120.75±11.63 |
0.006 |
|
5xSST |
14.24±4.78 |
16.88±5.88 |
0.026 |
|
Climbing
a ladder or step stool |
41% |
32% |
0.067 |
|
Carrying a shopping bag for a block |
75% |
57% |
0.032 |
|
Squatting |
43% |
22% |
0.002 |
|
Kneeling |
32% |
28% |
0.732 |
|
Running |
30% |
25% |
0.499 |
The TG reconstruction group had higher KSS scores compared to the control group at 6 weeks postoperatively (58.64±12.63 vs 53.18±11.40, p=0.039) and at 1 year postoperatively (86.03±10.35 vs 81.09±10.74, p=0.006). By 6 months postoperatively, there was a near statistically significant difference in KSS scores between the two groups (77.68 ± 11.63 vs 74.48 ± 15.01, p = 0.086) (Table 3) (Figure 8).

Table 3.
Comparison of KSS scores between the two groups.
|
Time |
TG reconstruction group |
Control group |
P Value |
|
2 weeks postoperative |
44.62±13.87 |
44.66±13.85 |
0.989 |
|
6 weeks postoperative |
58.64±12.63 |
53.18±11.40 |
0.039 |
|
3 months postoperative |
72.30±12.50 |
70.22±9.35 |
0.364 |
|
6 months postoperative |
77.68±11.63 |
74.48±15.01 |
0.086 |
|
1 year postoperative |
86.03±10.35 |
81.09±10.74 |
0.006 |
In terms of WOMAC scores, at 3 months postoperatively, the TG reconstruction group showed significant improvement over the control group in total WOMAC score (13.28 ± 10.38 vs 17.84 ± 7.48, p = 0.019), pain sub score (2.91 ± 1.99 vs 4.38 ± 2.49, p = 0.005), and physical function sub score (8.34 ± 8.78 vs 11.51 ± 5.72, p = 0.045). At 6 months postoperatively, the TG reconstruction group continued to show superiority in total WOMAC score (8.63 ± 7.24 vs 12.46 ± 11.13, p = 0.014) and physical function sub score (5.10 ± 5.42 vs 8.31 ± 8.38, p = 0.006). This advantage persisted at 1 year postoperatively in total WOMAC score (6.50 ± 6.64 vs 10.52 ± 10.23, p = 0.014) and physical function sub score (4.07 ± 4.53 vs 7.26 ± 7.82, p = 0.008). Even at 6 weeks postoperatively, the TG reconstruction group showed a trend towards better scores in the physical function sub score (12.95 ± 8.82 vs 16.45 ± 8.54, p = 0.059) (Table 4) (Figure 9).
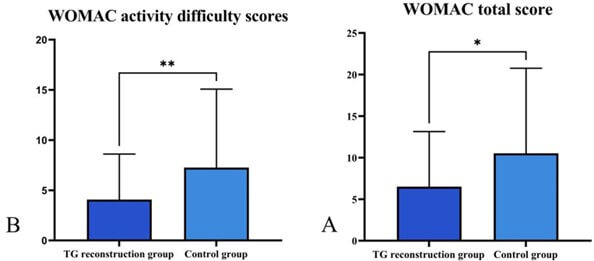
Table 4.
Comparison of WOMAC scores between the two groups.
|
|
TG reconstruction group |
Control group |
P Value |
|
2 weeks postoperative |
|
|
|
|
Total score |
37.05±14.46 |
36.98±17.12 |
0.98 |
|
Pain |
7.67±3.58 |
8.29±3.69 |
0.286 |
|
Stiffness |
3.23±1.35 |
3.2±1.54 |
0.901 |
|
Physical function |
26.15±11.76 |
25.46±13.31 |
0.733 |
|
6 weeks postoperative |
|
|
|
|
Total score |
20.27±11.64 |
23.11±10.56 |
0.223 |
|
Pain |
4.85±2.65 |
4.16±2.78 |
0.232 |
|
Stiffness |
2.48±0.90 |
2.69±0.88 |
0.266 |
|
Physical function |
12.95±8.82 |
16.45±8.54 |
0.059 |
|
3 months postoperative |
|
|
|
|
Total score |
13.28±10.38 |
17.84±7.48 |
0.019 |
|
Pain |
2.91±1.99 |
4.38±2.49 |
0.005 |
|
Stiffness |
2.03±0.86 |
2.00±0.96 |
0.880 |
|
Physical function |
8.34±8.78 |
11.51±5.72 |
0.045 |
|
6 months postoperative |
|
|
|
|
Total score |
8.63±7.24 |
12.46±11.13 |
0.014 |
|
Pain |
1.96±1.90 |
2.31±2.49 |
0.347 |
|
Stiffness |
1.57±0.96 |
1.84±1.21 |
0.144 |
|
Physical function |
5.10±5.42 |
8.31±8.38 |
0.006 |
|
1 year postoperative |
|
|
|
|
Total score |
6.50±6.64 |
10.52±10.23 |
0.014 |
|
Pain |
1.09±1.89 |
1.67±2.17 |
0.144 |
|
Stiffness |
1.34±1.10 |
1.6±1.12 |
0.241 |
|
Physical function |
4.07±4.53 |
7.26±7.82 |
0.008 |
In terms of SF-36, At 3 months postoperatively, the TG reconstruction group exhibited better scores in bodily pain, general health, and vitality compared to the control group. However, there were no significant differences between the two groups in any aspect of SF-36 scores at 6 months and 1 year postoperatively (Tables 5 & 6).
Table 5.
Comparison of SF-36 scores between the two groups (2 weeks postoperative, 6
weeks postoperative).
|
|
TG reconstruction group |
Control group |
P Value |
|
2 weeks postoperative |
|
|
|
|
Physical functioning |
37.57±18.16 |
35.96±24.30 |
0.732 |
|
Role-physical |
12.16±24.02 |
14.91±30.20 |
0.642 |
|
Bodily pain |
56.43±17.46 |
55.11±17.71 |
0.722 |
|
General health |
69.32±12.72 |
67.82±18.40 |
0.655 |
|
Vitality |
68.78±18.12 |
68.6±14.47 |
0.956 |
|
Social functioning |
64.86±16.09 |
64.25±18.05 |
0.868 |
|
Role-emotional |
34.15±32.77 |
30.47±29.19 |
0.569 |
|
Mental health |
74.59±13.34 |
76.21±17.60 |
0.635 |
|
Health transition |
32.43±15.43 |
40.79±22.47 |
0.051 |
|
6 weeks postoperative |
|
|
|
|
Physical functioning |
56.11±15.68 |
49.73±21.24 |
0.129 |
|
Role-physical |
31.94±39.91 |
26.39±38.54 |
0.516 |
|
Bodily pain |
61.72±13.40 |
57.24±13.41 |
0.128 |
|
General health |
76.13±15.19 |
65.58±20.61 |
0.005 |
|
Vitality |
71.92±16.24 |
67.18±22.07 |
0.262 |
|
Social functioning |
75.34±16.49 |
70.00±15.36 |
0.126 |
|
Role-emotional |
38.84±34.57 |
32.23±39.52 |
0.348 |
|
Mental health |
75.04±17.31 |
69.48±23.59 |
0.166 |
|
Health transition |
25.00±16.98 |
28.08±24.31 |
0.498 |
Table 6.
Comparison of SF-36 scores between the two groups (3 months postoperative, 6
months postoperative, and 1 year postoperative).
|
|
TG reconstruction group |
Control group |
P Value |
|
3 months postoperative |
|
|
|
|
Physical functioning |
63.53±22.54 |
55.66±19.79 |
0.056 |
|
Role-physical |
44.39±40.26 |
45.65±43.50 |
0.876 |
|
Bodily pain |
68.94±16.44 |
62.15±12.36 |
0.016 |
|
General health |
73.24±16.30 |
65.44±18.49 |
0.025 |
|
Vitality |
72.25±20.50 |
62.42±22.95 |
0.018 |
|
Social functioning |
71.46±20.35 |
67.33±19.25 |
0.285 |
|
Role-emotional |
60.08±32.64 |
57.32±39.92 |
0.703 |
|
Mental health |
72.78±16.21 |
66.30±22.85 |
0.104 |
|
Health transition |
28.80±33.73 |
25.79±28.02 |
0.612 |
|
6 months postoperative |
|
|
|
|
Physical functioning |
66.59±19.16 |
66.25±21.29 |
0.939 |
|
Role-physical |
72.11±39.96 |
70.00±43.19 |
0.816 |
|
Bodily pain |
76.89±9.62 |
77.13±10.67 |
0.914 |
|
General health |
67.69±15.63 |
65.25±16.96 |
0.492 |
|
Vitality |
68.84±17.11 |
67.63±19.41 |
0.759 |
|
Social functioning |
79.00±19.72 |
80.62±19.80 |
0.706 |
|
Role-emotional |
79.41±32.70 |
75.75±37.69 |
0.634 |
|
Mental health |
70.60±20.29 |
72.20±20.53 |
0.719 |
|
Health transition |
23.86±24.68 |
27.50±25.19 |
0.506 |
|
1 year postoperative |
|
|
|
|
Physical functioning |
66.91±16.68 |
67.63±20.32 |
0.844 |
|
Role-physical |
69.49±39.31 |
69.74±43.16 |
0.976 |
|
Bodily pain |
76.66±9.28 |
77.50±10.60 |
0.673 |
|
General health |
70.12±15.77 |
65.39±16.64 |
0.150 |
|
Vitality |
71.91±14.78 |
69.47±18.29 |
0.457 |
|
Social functioning |
90.99±22.63 |
91.44±20.97 |
0.919 |
|
Role-emotional |
78.35±32.42 |
76.23±37.85 |
0.763 |
|
Mental health |
73.00±19.85 |
73.47±20.96 |
0.908 |
|
Health transition |
19.85±23.08 |
25.00±25.33 |
0.290 |
One patient in the experimental group experienced early periprosthetic joint infection, which was resolved after debridement and liner exchange. No further infections occurred during follow-up. No further infections occurred during follow-up. Two patients in the experimental group and two in the control group experienced delayed wound healing postoperatively, which improved after outpatient wound care. There were no significant differences between the two groups in terms of postoperative complications at 1 year postoperatively (Table 7).
Table
7. Incidence of
postoperative complications.
|
Adverse events |
TG reconstruction group (N) |
Control group (N) |
P Value |
|
Prosthetic joint infection |
1 |
0 |
0.314 |
|
Poor wound healing |
2 |
2 |
0.992 |
|
Total |
3 |
2 |
0.624 |
4. Discussion
By preoperative planning, we personalized the rotation of the femoral component and reconstructed the preoperative trochlear groove. Our study results demonstrate that this personalized preoperative planning can improve knee joint function in patients, particularly evident in advanced activities such as squatting. Lisa Spahn Lundgren et al.'s research indicates that in robot-assisted total knee arthroplasty (TKA), surgical planning, especially femoral component alignment and rotation, significantly affects postoperative joint function [22]. Personalized surgical planning has been shown to be beneficial [22].
Our research results also show that, by reconstructing the patellar groove trajectory of patients, the postoperative patellofemoral index and patellar tilt angle of patients in the TG reconstruction group are better than those in the control group. In preoperative planning, we focus on matching the prosthetic patellar groove with the patient's original patellar groove to restore the patient's original patellar groove morphology, referred to as the "kinematic patellofemoral line". This may enable patients in the experimental group to achieve a more "native" patellar trajectory, thereby improving their joint function and range of motion.
Knee joint range of motion is a critical indicator of postoperative joint function in TKA [27] and significantly influences patient-reported outcomes [28]. Yang Yang et al.'s study results suggest that robot assisted TKA outperforms traditional surgery in knee joint range of motion at 6 months postoperatively (118.5° vs 112.2°) [29]. Yunus Demirtas et al. demonstrated that at 1 year postoperatively, patients undergoing robot assisted TKA achieved a knee joint range of motion of 125.2° [30], which is similar to our study. The rotation of the femoral component will affect the patellar stress, thereby significantly influencing knee joint function and range of motion [31, 32], even a 2.5 mm displacement can lead to a 20° change in knee joint range of motion [33]. Although robot-assisted total knee arthroplasty can provide more precise alignment, it may not necessarily lead to better results in terms of postoperative function and joint range of motion [33]. Therefore, a more individualized alignment of the component, rather than a uniform alignment standard, may be a further solution. We believe that setting individualized rotational alignment for each patient to restore their trochlear groove morphology may lead to higher joint function. As shown in (Figure 2), the distribution of the femoral component relative to the transepicondylar axis rotation angle is quite wide, not a fixed value, highlighting the importance of individualized surgical plans.
Squatting is a key indicator of high flexion knee joint activity [34]. Aditya K Aggarwal et al. found that on average, 17% of patients could squat at an average of 5.5 years postoperatively [26]. Matthew S Hepinstall et al. reported that 41% of patients could squat at 1 year postoperatively [34]. Our study shows that at 1 year postoperatively, 43% of patients in the experimental group could squat, slightly better than previous studies. This improvement may be attributed to our personalized preoperative planning, which restored the patellofemoral status to preoperative conditions, thereby enhancing joint function. Periklis Tzanetis et al. demonstrated that appropriate adjustments in preoperative planning can help maximize the restoration of pre-disease joint status [35], aligning with our research concept. Additionally, our study results show that at 1 year postoperatively, the TG reconstruction group had higher KSS scores than the control group, with a statistically significant difference greater than the clinical minimal difference (5 points) [36]. In terms of WOMAC scores, the experimental group outperformed the control group at 6 months and 1 year postoperatively. The score differences between the two groups mainly stemmed from difficulties in physical function. This suggests that patients in the experimental group had better joint function, though there were no significant differences in pain and stiffness scores between the groups.
In the 5xSST, the experimental group performed better than the control group, although the difference did not reach the minimum clinically important difference (3 seconds) [37]. Regarding SF-36 scores, the TG reconstruction group was superior to the control group at 6 weeks postoperatively, indicating a potential early recovery advantage. However, there were no significant differences in SF-36 scores between the two groups at 1 year postoperatively.
Our study also has limitations. First, we did not study postoperative patellar trajectory in patients. Second, we only included patients undergoing MAKO robot-assisted TKA, and further research should encompass more robotic-assisted systems. Third, our follow-up duration was relatively short, necessitating longer-term observations to evaluate patient joint function and prosthetic status.
5. Conclusion
Our study found that personalized adjustment of the femoral component rotation angle using robot-assisted total knee arthroplasty restores the patient's physiological trochlear groove morphology, leading to improved joint function. This underscores the importance of personalized preoperative planning in robot-assisted total knee arthroplasty.
Conflicts of Interest
None.
Funding
National Natural Science Foundation of China: 82272558.
REFERENCES
[1] A D Boyd Jr, F C Ewald, W H Thomas,
et al. “Long-term complications after total knee arthroplasty with or without
resurfacing of the patella.” J Bone Joint Surg Am, vol. 75, no. 5, pp.
674-681, 1993. View at: Publisher Site | PubMed
[2] J T Chew, N J Stewart, A D Hanssen,
et al. “Differences in patellar tracking and knee kinematics among three
different total knee designs.” Clin Orthop Relat Res, no. 345, pp.
87-98, 1997. View at: PubMed
[3] M L Clayton, R Thirupathi “Patellar
complications after total condylar arthroplasty.” Clin Orthop Relat Res,
no. 170, pp. 152-155, 1982. View at: PubMed
[4] A F Lynch, C H Rorabeck, R B Bourne
“Extensor mechanism complications following total knee arthroplasty.” J
Arthroplasty, vol. 2, no. 2, pp. 135-140, 1987. View at: Publisher Site | PubMed
[5] J R Moreland “Mechanisms of failure
in total knee arthroplasty.” Clin Orthop Relat Res, no. 226, pp. 49-64.
1988. View at: PubMed
[6] R L Merkow, M Soudry, J N Insall
“Patellar dislocation following total knee replacement.” J Bone Joint Surg
Am, vol. 67, no. 9, pp. 1321-1327, 1985. View at: PubMed
[7] J N Grace, J A Rand “Patellar
instability after total knee arthroplasty.” Clin Orthop Relat Res, no.
237, pp. 184-189, 1988. View at: PubMed
[8] H E Figgie 3rd 1, V M Goldberg, M P
Figgie, et al “The effect of alignment of the implant on fractures of the
patella after condylar total knee arthroplasty.” J Bone Joint Surg Am,
vol. 71, no. 7, pp. 1031-1039, 1989. View at: PubMed
[9] G W Brick, R D Scott “The
patellofemoral component of total knee arthroplasty.” Clin Orthop Relat Res,
no. 231, pp. 163-178, 1988. View at: PubMed
[10] Arnd Steinbrück, Christian Schröder,
Matthias Woiczinski, et al. “The effect of trochlea tilting on patellofemoral
contact patterns after total knee arthroplasty: an in vitro study.” Arch
Orthop Trauma Surg, vol. 134, no. 6, pp. 867-872, 2014. View at: Publisher Site | PubMed
[11] Wolf Petersen, Ingo Volker Rembitzki,
Gerd-Peter Brüggemann, et al. “Anterior knee pain after total knee
arthroplasty: a narrative review.” Int Orthop, vol. 38, no. 2, pp.
319-328, 2014. View at: Publisher
Site | PubMed
[12] Ghias Bhattee, Pradeep Moonot, Raj
Govindaswamy, et al. “Does malrotation of components correlate with patient
dissatisfaction following secondary patellar resurfacing?” Knee, vol.
21, no. 1, pp. 247-251, 2014. View at: Publisher Site | PubMed
[13] Takashi Terashima, Tomohiro Onodera,
Naohiro Sawaguchi, et al. “External rotation of the femoral component decreases
patellofemoral contact stress in total knee arthroplasty.” Knee Surg Sports
Traumatol Arthrosc, vol. 23, no. 11, pp. 3266-3272, 2015. View at: Publisher Site | PubMed
[14] C Verlinden, P Uvin, L Labey, et al.
“The influence of malrotation of the femoral component in total knee
replacement on the mechanics of patellofemoral contact during gait: an in vitro
biomechanical study.” J Bone Joint Surg Br, vol. 92, no. 5, pp. 737-742,
2010. View at: Publisher
Site | PubMed
[15] Kars P Valkering, Stefan J Breugem,
Michel Pj van den Bekerom, et al. “Effect of rotational alignment on outcome of
total knee arthroplasty.” Acta Orthop, vol. 86, no. 4, pp. 432-439,
2015. View at: Publisher
Site | PubMed
[16] Matthias Woiczinski, Manuel Kistler,
Christian Schröder, et al. “TKA design-integrated trochlea groove rotation
reduces patellofemoral pressure.” Knee Surg Sports Traumatol Arthrosc,
vol. 27, no. 5, pp. 1680-1692, 2019. View at: Publisher Site | PubMed
[17] Tadashi Tsukeoka, Yoshikazu
Tsuneizumi “Postoperative femoral component rotation using posterior condylar
referencing is difficult to predict preoperatively in total knee arthroplasty.”
Knee, vol. 41, pp. 380-388, 2023. View at: Publisher Site | PubMed
[18] Simon Talbot, Pandelis Dimitriou,
Michael Mullen, et al. “Referencing the sulcus line of the trochlear groove and
removing intraoperative parallax errors improve femoral component rotation in
total knee arthroplasty.” Knee Surg Sports Traumatol Arthrosc, vol. 25,
no. 9, pp. 2743-2750, 2017. View at: Publisher Site | PubMed
[19] Pietro Cerveri 1, Mario Marchente,
Alfonso Manzotti, et al. “Determination of the Whiteside line on femur surface
models by fitting high-order polynomial functions to cross-section profiles of
the intercondylar fossa.” Comput Aided Surg, vol. 16, no. 2, pp. 71-85,
2011. View at: Publisher
Site | PubMed
[20] Susanne Fuchs 1, Adrian Skwara,
Carsten O Tibesku, et al. “Retropatellar contact characteristics before and
after total knee arthroplasty.” Knee, vol. 12, no. 1, pp. 9-12, 2005.
View at: Publisher
Site | PubMed
[21] Theofilos Karasavvidis, Cale A Pagan,
Eytan M Debbi, et al. “No Difference in Limb Alignment Between Kinematic and
Mechanical Alignment Robotic-Assisted Total Knee Arthroplasty.” J
Arthroplasty. View at: Publisher
Site | PubMed
[22] Lisa Spahn Lundgren, Nathalie
Willems, Robert C Marchand, et al. “Surgical factors play a critical role in
predicting functional outcomes using machine learning in robotic-assisted total
knee arthroplasty.” Knee Surg Sports Traumatol Arthrosc. View at: Publisher Site | PubMed
[23] Cécile Batailler, Andrea Fernandez,
John Swan, et al. “MAKO CT-based robotic arm-assisted system is a reliable
procedure for total knee arthroplasty: a systematic review.” Knee Surg
Sports Traumatol Arthrosc, vol. 29, no. 11, pp. 3585-3598, 2021. View at: Publisher Site | PubMed
[24] Nanne Kort, Patrick Stirling, Peter
Pilot “Robot-assisted knee arthroplasty improves component positioning and
alignment, but results are inconclusive on whether it improves clinical scores
or reduces complications and revisions: a systematic overview of
meta-analyses.” Knee Surg Sports Traumatol Arthrosc, vol. 30, no. 8, pp.
2639-2653, 2022. View at: Publisher
Site | PubMed
[25] Christopher W Jones, Seth A Jerabek
“Current Role of Computer Navigation in Total Knee Arthroplasty.” J
Arthroplasty, vol. 33, no. 7, pp. 1989-1993, 2018. View at: Publisher Site | PubMed
[26] Aditya K Aggarwal, Anuj Agrawal
“Mobile vs fixed-bearing total knee arthroplasty performed by a single surgeon:
a 4- to 6.5-year randomized, prospective, controlled, double-blinded study.” J
Arthroplasty, vol. 28, no. 10, pp. 1712-1716, 2013. View at: Publisher Site | PubMed
[27] Victoria Ko, Justine Naylor, Ian
Harris, et al. “One-to-one therapy is not superior to group or home-based
therapy after total knee arthroplasty: a randomized, superiority trial.” J
Bone Joint Surg Am, vol. 95, no. 21, pp. 1942-1949, 2013. View at: Publisher Site | PubMed
[28] Jean-Noel Argenson, Sebastien
Parratte, Abdullah Ashour, et al. “Patient-reported outcome correlates with
knee function after a single-design mobile-bearing TKA.” Clin Orthop Relat
Res, vol. 466, no. 11, pp. 2669-2676, 2008. View at: Publisher Site | PubMed
[29] Yang Yang, Lingjun Jiang, Xiaoxiao
Zhou, et al. “Robotic-assisted total knee arthroplasty improves implant
position and early functional recovery for the knee with severe varus/valgus
deformity.” BMC Musculoskelet Disord, vol. 25, no. 1, pp. 92, 2024. View
at: Publisher
Site | PubMed
[30] Yunus Demirtas, Abdulsamet Emet,
Gokhan Ayik, et al. “A novel robot-assisted knee arthroplasty system (ROSA) and
1-year outcome: A single center experience.” Medicine (Baltimore), vol.
102, no. 42, pp. e35710, 2023. View at: Publisher Site | PubMed
[31] Mouhanad M El-Othmani, Abdul K
Zalikha, Roshan P Shah “Anterior Knee Pain After Total Knee Arthroplasty: A
Critical Review of Peripatellar Variables.” JBJS Rev, vol. 11, no. 7,
2023. View at: Publisher
Site | PubMed
[32] David Shervin, Katelyn Pratt, Travis
Healey, et al. “Anterior knee pain following primary total knee arthroplasty.” World
J Orthop, vol. 6, no. 10, pp. 795-803, 2015. View at: Publisher Site | PubMed
[33] Olga Adamska, Krzysztof Modzelewski,
Jakub Szymczak, et al. “Robotic-Assisted Total Knee Arthroplasty Utilizing
NAVIO, CORI Imageless Systems and Manual TKA Accurately Restore Femoral
Rotational Alignment and Yield Satisfactory Clinical Outcomes: A Randomized
Controlled Trial.” Medicina (Kaunas), vol. 59, no. 2, pp. 236, 2023.
View at: Publisher
Site | PubMed
[34] Matthew S Hepinstall, Amar S Ranawat,
Chitranjan S Ranawat “High-flexion total knee replacement: functional outcome
at one year.” HSS J, vol. 6, no. 2, pp. 138-144, 2010. View at: Publisher Site | PubMed
[35] Periklis Tzanetis, René Fluit, Kevin
de Souza, et al. “Pre-Planning the Surgical Target for Optimal Implant
Positioning in Robotic-Assisted Total Knee Arthroplasty.” Bioengineering
(Basel), vol. 10, no. 5, pp. 543, 2023. View at: Publisher Site | PubMed
[36] Filippo Migliorini, Nicola Maffulli, Luise Schäfer, et al. “Minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient-acceptable symptom state (PASS) in patients who have undergone total knee arthroplasty: a systematic review.” Knee Surg Relat Res, vol. 36, no. 1, pp. 3, 2024. View at: Publisher Site | PubMed
[37] Rodrigo Martín-San Agustín, Mª José Crisostomo, Mª Piedad Sánchez-Martínez, et al. “Responsiveness and Minimal Clinically Important Difference of the Five Times Sit-to-Stand Test in Patients with Stroke.” Int J Environ Res Public Health, vol. 18, no. 5, pp. 2314, 2021. View at: Publisher Site | PubMed