Received: Wed 14, May 2025
Accepted: Fri 06, Jun 2025
Abstract
Introduction: Acute appendicitis is a frequently encountered emergency in general surgery. However, an atypical position of the appendix can complicate the diagnosis and surgical approach. Retroperitoneal positioning of the appendix is a rare anatomical variant that may mimic other abdominal or renal conditions.
Case Report: We report a case of a 21-year-old male presenting with right flank pain and vomiting. Examination showed right iliac fossa tenderness without classical signs of peritonitis. Laboratory parameters were largely normal, and abdominal ultrasound did not visualize the appendix. Due to persistent symptoms, a laparoscopic exploration was planned. Intraoperatively, the appendix was located retroperitoneally after mobilization of the cecum and was inflamed. A retrograde appendectomy was performed successfully. Histopathology confirmed acute appendicitis.
Conclusion: Retroperitoneal appendicitis, though rare, should be considered in patients presenting with atypical right-sided abdominal pain. Surgical exploration and awareness of anatomical variations are essential for accurate diagnosis and treatment.
Keywords
Retroperitoneal appendix, retrograde appendectomy, atypical appendicitis
1. Introduction
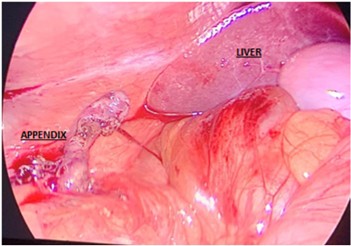
Appendicitis is one of the most common indications for emergency abdominal surgery. Although the appendix typically lies in the right iliac fossa, various positional anomalies can occur, including retrocecal, subhepatic, pelvic, and retroperitoneal locations. Retroperitoneal appendix is particularly rare and can present diagnostic challenges due to atypical clinical features and inconclusive imaging.
2. Case Report
A 21-year-old unmarried male presented with severe right flank pain and three episodes of vomiting over the last 24 hours. The pain was continuous, with acute intermittent exacerbations, radiating to the back, and was not relieved by over-the-counter analgesics. He had no similar episodes in the past.
On clinical examination, the patient was afebrile with a pulse of 96 bpm and blood pressure of 130/70 mmHg. SpO2 dropped to 90% during acute spasms. Abdominal examination showed right iliac fossa tenderness without rebound tenderness or guarding. The remainder of the examination was unremarkable.
Lab tests revealed hemoglobin 11.4 g/dL, WBC 7,500/mm³ (51% neutrophils, 49% lymphocytes), and 3-5 pus cells per high-power field in urine. Ultrasound of the abdomen showed no localized fluid collection and did not visualize the appendix. CT imaging was unavailable at this remote location. A working diagnosis of right ureteric colic was made with acute appendicitis and urinary tract infection as a differential. The patient was admitted and managed conservatively with intravenous fluids, antibiotics, and analgesics. However due to persistent symptoms even after 24 hrs of onset, despite medical management, suspicion of appendicular pathology grew stronger and a diagnostic laparoscopy was planned.
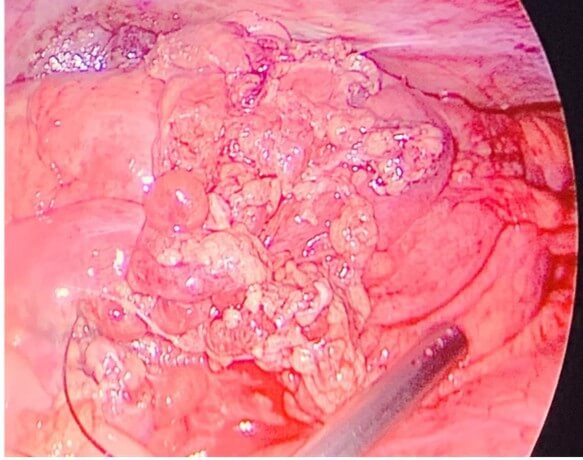
Intraoperatively, the right iliac fossa had multiple enlarged lymph nodes, minimal fluid collection was noted, but the appendix was not found in its usual location. Missing appendix in its routine location led us to the initial identification of ascending colon and tracing down to the caecal base. In an attempt to identify the base of caecum, mobilisation of the cecum was done by incising the right lateral peritoneal reflection. The tip of the appendix was seen emerging behind the peritoneal fold and eventually an inflamed, 8 cm retroperitoneal, edematous appendix was identified. A retrograde appendectomy was performed. The base was healthy. No drain was placed. Postoperative recovery was uneventful. Histopathological examination confirmed acute appendicitis with congested vessels and infiltration of inflammatory cells.
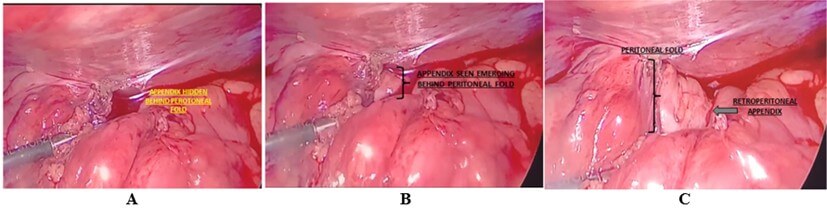
A) Initial exploration of the retroperitoneum. B) Progressive mobilization revealing the appendix. C) Complete exposure of the appendix from behind the fold.
3. Discussion
3.1. Patient Characteristics
Retroperitoneal appendicitis remains a rare and diagnostically challenging variant of a common surgical emergency. Its presentation often mimics renal or musculoskeletal conditions due to its posterior location, leading to potential delays in diagnosis and treatment. Recent literature emphasizes the importance of considering positional anomalies of the appendix when patients present with atypical abdominal or flank pain. A 2023 systematic review by Zhang et al. noted that retroperitoneal appendicitis accounted for fewer than 0.3% of appendectomy cases, with most presenting with non-classical symptoms such as back or right flank pain, often mistaken for urolithiasis or psoas abscesses [2].
Ultrasound frequently fails to visualize the appendix in these cases, as was true in our patient. Computed tomography (CT) remains the gold standard for diagnosis, especially in resource-rich settings. A multicenter retrospective study by Almeida et al. (2023) reinforced the diagnostic accuracy of CT in detecting retrocecal and retroperitoneal appendicitis, suggesting its integration in persistent right lower quadrant pain of unclear origin [3]. However, limited access to imaging in low-resource settings, like in our case, necessitates reliance on clinical judgment and exploratory surgery. Surgical management also requires tailored approaches. Retrograde appendectomy, as performed in our case, is particularly suited when the tip is more accessible than the base. A recent technical note by López-Rodríguez et al. (2024) supports this approach for atypically located appendices, highlighting reduced operative time and comparable postoperative outcomes [4].
Intraoperative exploration, including mobilization of the cecum, is critical for identifying retroperitoneal appendices. Surgeons should maintain a high index of suspicion in patients with persistent symptoms despite normal laboratory and sonographic findings. Retroperitoneal appendicitis is an uncommon entity and poses significant diagnostic challenges. Its presentation often overlaps with renal or musculoskeletal pathologies, especially when flank or back pain predominates. In our case, the inability to visualize the appendix on ultrasound and atypical symptoms necessitated exploration. While CT scan is the diagnostic tool of choice in such scenarios, remote areas with limited resources and financial limitations preclude its use. Intraoperative mobilization of the cecum was crucial to identifying the appendix. Retrograde appendectomy is a well-accepted surgical approach when the tip of the appendix is first located, especially in such anomalous positions.
4. Conclusion
Though rare, retroperitoneal appendix should be considered in differential diagnosis when patients present with right-sided abdominal or flank pain unresponsive to conservative management. Awareness and timely surgical intervention are key to favorable outcomes.
Ethical Statement
Informed consent was obtained from the patient for publication of this case report and accompanying images.
REFERENCES
[1]
Sulu B, Gunerhan Y, Palanci Y, et al.
“Retroperitoneal appendicitis: an uncommon presentation of a common disease.” Am
J Emerg Med, vol. 28, no. 1, pp. 115.e3-115.e5, 2010.
[2]
Zhang Y, Wang S, Huang X “Atypical presentations of
appendicitis: A systematic review of retrocecal and retroperitoneal cases.” Surg
Pract, vol. 27, no. 1, pp. 14-22, 2023.
[3]
Almeida J, Rao P, Nair S “Diagnostic yield of CT in
appendicitis with anatomical variants: A multicenter retrospective analysis.” J
Surg Res, vol. 284, pp. 156-162, 2023.
[4] López-Rodríguez JL, Mehta D, Bhandari M “Retrograde appendectomy for posteriorly located appendices: A technical perspective.” Int J Surg Case Rep, vol. 107, pp. 108032, 2024.
