Received: Wed 08, May 2024
Accepted: Tue 16, Jul 2024
Abstract
Background: Knee arthroplasty, also knowns as knee replacement surgery, is a procedure commonly performed to relieve pain and improve function in individuals with severe end-stage knee osteoarthritis (OA), commonly primary OA or secondary, due to previous trauma or rheumatoid arthritis. Knee arthroplasty can be defined as: uni-compartmental knee arthroplasty (UKA) for either medial or lateral sides; patellofemoral joint replacement (PFJR) or total knee arthroplasty (TKA). Internal fixation for various scenarios occurring in knee arthroplasty have been reported in literature. The aim of this study was to quantify the incidence and any patient specific patterns in which early internal fixation was used for peri-prosthetic fractures or other causes occurring most likely at the time of index arthroplasty surgery or in the early perioperative period. Peri-prosthetic fractures around the knee are well documented, but there is limited literature available about the specific management and outcomes of intra-operative and occult fractures occurring in the early post-operative period in a large consecutive patient cohort. Currently there is no consensus about optimal treatment of these types of fractures.
Methods: Data from a consecutive single institution cohort of primary knee arthroplasty patients was analyzed to determine patients who had early internal fixations following primary knee arthroplasty either intraoperatively or in the early perioperative period. The basic demographics of this group, the type and time of fixation used, and early outcomes was then defined.
Results: Of 8,453 patients undergoing primary knee arthroplasty, we identified 13 cases in which internal fixation techniques were used. In five cases, an intra-operative fracture occurred requiring immediate fixation. Another five cases were diagnosed with an occult fracture in the early post-operative period despite a normal post-operative overview radiography. Three other cases where internal fixation was used for causes other than a peri-prosthetic fracture.
Conclusion: A small proportion of patients undergoing primary knee arthroplasty may need acute internal fixation during or shortly after surgery for various indications. Therefore, retaining the skill set of internal fixation techniques remains important. Locking compression plate (LCP) fixation for these cases appears to be more useful than limited non-locking plating or isolated screw fixation.
Keywords
Knee arthroplasty, internal fixation, early ORIF in knee arthroplasty, periprosthetic fractures
1. Introduction
Knee arthroplasty, also known as knee replacement surgery, is a well-known, cost-effective orthopedic procedure used to treat severe knee joint pain and disability, typically caused by conditions such as osteoarthritis, rheumatoid arthritis, or traumatic injuries. During knee arthroplasty, the damaged or worn-out parts of the knee joint are replaced with artificial components, which are designed to replicate the function of a healthy knee joint. Knee arthroplasty involves unicondylar knee arthroplasty (UKA), total knee arthroplasty (TKA) or patellofemoral joint replacement (PFJR). In the United Kingdom the NJR recorded 100,547 primary TKRs in 2018. The projections of overall numbers of primary TKRs in UK will be 118,503 in 2030, 128,849 in 2040, 133,789 in 2050 and 137,341 in 2060. By 2060, it is estimated that there would be a 36.6% increase in the number of primary TKRs compared with 2018 [1]. Intraoperative fractures in revision knee arthroplasty have been well documented but literature on these in primary knee arthroplasty is limited. Intra-operative occurrence of a fracture is a rare but recognized complication in primary knee arthroplasty surgery, with an incidence of 0.2 - 4.4% with higher risks associated with rheumatoid arthritis, osteoporosis, older age, female gender, chronic steroid uses, metabolic disorders, PS type femoral implants and difficult surgical exposure due to severe coronal/sagittal plane deformities of the knee [2].
Cases of occult fractures in the early post-operative period after UKA and TKA without history of trauma have been reported as well. Additional surgery for internal fixation is needed in these cases to reduce and stabilize these types of fractures upholding the standard principles of fracture fixation and arthroplasty principles at the same time. Therefore, retaining the skillset of internal fixation techniques within the arthroplasty department remains important. However, there might be more indications in which internal fixation techniques are being used. Additional situations where internal fixation implants and techniques have a role are occult fractures, pre-operative insufficiency proximal tibia fracture, deformity correction with realignment osteotomy and for neutralizing stress riser in inter-prosthetic constructs.
2. Material and Methodology
A case series study was performed to examine the application of internal fixations in primary knee arthroplasty. To collect data on all primary knee arthroplasty, the hospital’s operative database of all primary knee arthroplasties was retrieved using the OPCS 4 codes of W410 to W520. This database covered a sixteen-year period from 2003 to 2018. During this timeframe, the two main primary total knee arthroplasties (TKA) used were the Triathlon (Stryker, Newbury UK) and the Nexgen (Zimmer-Biomet, Swindon UK) and the main uni-compartmental knee arthroplasty (UKA) was the Oxford (Zimmer-Biomet, Brigend UK).
Inclusion criteria consisted of all patients who had internal fixation devices implanted along with knee arthroplasty implants in the following situations:
i) Intraoperative fractures.
ii) Occult fractures which manifested as early peri-prosthetic fractures following knee arthroplasty and operated within 42 days of the index surgery.
iii) Stabilization of an intraoperative realignment osteotomy for deformity correction occurring at the time of the arthroplasty.
iv) Neutralizing stress risers at the inter-prosthetic region.
Exclusion from the study were:
i) A peri-prosthetic fracture treated more than 42 days post-index arthroplasty operation.
ii) A fracture occurring in a patient having had their surgery in another institution.
iii) A fracture occurring peri-operatively in a revision knee replacement.
iv) A peri-prosthetic fracture treated non-operatively were excluded.
2.3. Statistical Analysis
Subsequently, a request was made to the database to seek out OPCS codes related to open reduction internal fixation of long bones in conjunction with primary knee arthroplasties. Additionally, the department’s complication audit database was utilized to pinpoint patients who had experienced fractures.
In the selected cohort, we conducted an overlook in patient report of basic demographics, osteoarthritis pattern (deformity and bone loss), evidence of documented osteoporosis, fracture location and type, time to diagnose, time to treatment, type of treatment, outcome in early and post-operative periods based on subjective and objective parameters and standard patient related outcome measures (PROMs), additional complications within 42 days.
3. Results
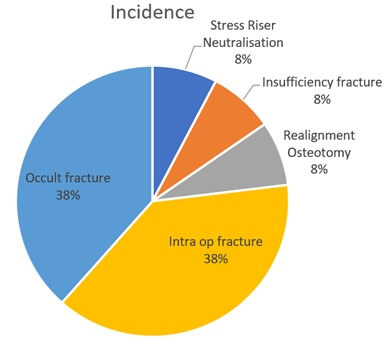
A total of 8,453 primary knee arthroplasties, including unicondylar knee replacement (UKR), total knee replacement (TKA) performed in one institution from 2003 to 2018, were evaluated for the use of internal fixation during or within 6 weeks of knee arthroplasty. We found 13 cases (0.001%) which fitted the inclusion criteria. In five cases internal fixation was performed to stabilize an intra-operative fracture during knee arthroplasty. In five cases, delayed diagnosis of intra-operative occult fractures without history of trauma lead to re-surgery in the early post-operative period. In one case internal fixation was done to address a post traumatic varus deformity of the distal femur, concurrently with a TKA. There was one case of insufficiency fracture of proximal tibia sustained one week before the scheduled TKA in a patient with severe osteo-arthritis needing internal fixation along with the arthroplasty. In one patient we used internal fixation for neutralizing stress riser in an inter-prosthetic construct. A summary of the cases is shown in (Figure 1).
Techniques for internal fixation varied amongst type of fracture and choice of the surgeon. In one case, a tibial intra-operative fracture was treated with 4 mm cannulated cancellous screws. Six cases were treated with tibial locked compression plates (LCP) and three with a tubular non-locked plate. In one case, TKA was combined with deformity corrective osteotomy and final stabilization with dual distal femur locking plates and autologous bone grafting.
Of the 13 patients, twelve were females and one was male. The median age of the group was 73 years, ranging from 62 to 85 years. Detailed demographics of the entire cohort is in (Table 1).
Table 1. Summary of the 13 cases,
which involved the concurrent use of internal fixation devices in the early
peri-operative phase of TKA.
|
Patient |
Age year / sex |
Knee Arthroplasty type |
Indication for Internal Fixation |
Internal Fixation Implant used |
Time of ORIF operation |
Follow-up period |
|
1 |
63 / F |
TKR |
Intra-operative fracture |
AxSOS
3 proximal tibia medial LCP |
0: with TKR |
5 years |
|
2 |
67 / F |
Medial UKR |
Intra-operative fracture |
4mm Cannulated cancellous screws |
0: with TKR |
10 years |
|
3 |
84 / M |
TKR |
Intra-operative fracture |
Tibial 1/3 tubular non-locked
plate |
0: with TKR |
1 year |
|
4. |
69 / F |
TKR |
Intra-operative fracture |
Tibial 1/3 tubular non-locked plate |
0: with TKR |
2 year |
|
5 |
69 / F |
TKR |
Intra-operative fracture |
1/3 tubular non locked plate +
stem extension |
0: with TKR |
6 months
|
|
6 |
71/ F |
Medial UKR |
Occult fracture |
AxSOS 3 proximal tibia medial LCP |
11 days |
8 months |
|
7 |
71 / F |
Medial UKR |
Occult fracture |
AxSos 3 proximal tibial plate |
35 days |
2 years |
|
8 |
89 / F |
Medial UKR |
Occult fractur |
AxSOS 3 proximal tibia medial LCP |
10 days |
1 year |
|
9 |
70/F |
Medial UKR |
Occult fracture |
AxSOS 3 proximal tibia medial LCP
|
21days |
1 year |
|
10 |
82 / F |
TKR |
Occult fracture |
AxSOS 3 distal lateral femur LCP |
12 days |
6 years |
|
11 |
79/ F |
TKR |
Pre-operative insufficiency
proximal tibia fracture |
Medial proximal tibia 3,5 mm
AxSOS plate LCP |
0: with TKR |
2 years |
|
12 |
69/F |
TKR |
Deformity correction with realignment osteotomy |
AxSOS 3 medial & lateral distal femur LCP |
0: with TKR |
1 year |
|
13 |
67/F |
TKR |
Neutralising stress risers |
AxSOS 3 lateral distal femur LCP |
0: with TKR |
1 year |
F: Female; M: Male; TKR:
Total Knee Replacement; UKR: Unicondylar Knee Replacement; LCP: Locking
Compression Plate.
3.1. Intraoperative Fractures (n= 5)
An intraoperative medial tibial condyle fracture occurred intra-operatively in a primary TKA for which AxSOS 3 Titanium Locked compression plate 3.5 system (Stryker, Switzerland) was used. It occurred due to a technical error of tibial tray placement, which was removed and re-implanted. This led to a posteromedial tibial plateau fracture which was stabilized by a proximal tibia locked compression plate. The subject had a follow-up of 5 years and the fracture healed uneventfully. The patient experienced significant and persistent post-operative pain, with elements of neuropathic pain early on, up to time of last follow-up.
A tibial spine avulsion, including the ACL footprint, occurred once in our series, in a medial UKA case while taking the knee through the range of movement following implant placement. A 4 mm cannulated cancellous screw was used to fix this. The avulsion fracture healed uneventfully. The patient went on to undergo total knee arthroplasty due to progressive lateral compartmental osteoarthrits at 10 years post index surgery.
3.2. Occult Fractures (n=5)
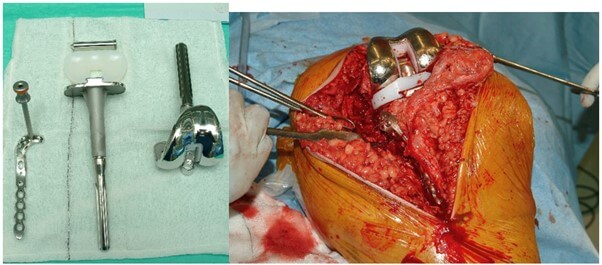
Our cohort of cases had five occult fractures, which likely occurred during the surgical procedure, but were identified at a later stage in the postoperative period. Among the patients in this subgroup, four out of five had previously undergone a medial UKA, and these fractures manifested as early peri-prosthetic fractures during the recovery phase (Figure 2). Most of these patients were able to bear full weight immediately after surgery. However, they were diagnosed due to persistent pain, lack of improvement, and early follow-up X-rays. Notably, two out of the five patients had normal early postoperative radiographs.
The mean time for the presentation of this subtype of "early" peri-prosthetic fractures was 17.8 days, with a range of 10 to 35 days. All fractures associated with UKA healed without complications following proximal tibial plating using AxSOS (Stryker, Newbury UK), leading to positive outcomes (Figure 3). In the case of a TKA with an early peri-prosthetic fracture, distal femur locked compression plating was employed. This patient experienced a superficial postoperative infection, which was successfully managed with intravenous antibiotics without the need for further surgical intervention. The patient was followed for a period of 6 years and eventually healed without any significant complications.


3.3. Insufficiency Fracture of Tibia with Knee Osteoarthritis (n=1)
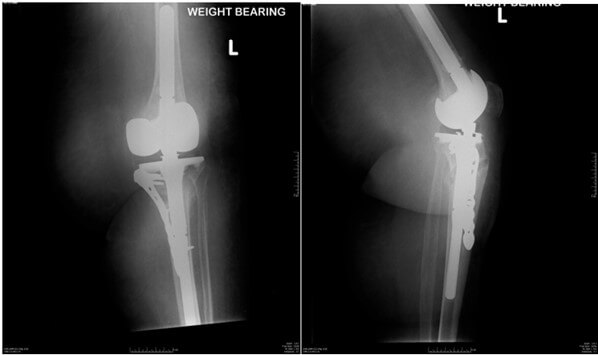
We had a single case of a patient who presented acutely one week prior to her planned elective TKR date with an insufficiency fracture of the proximal tibia with underlying knee osteoarthritis (Figure 4) for which primary total knee arthroplasty was done with a proximal tibial LCP, with autologous bone graft from the TKA cuts (Figures 5 & 6). The patient was followed up for 2 years and she had an uneventful recovery with good range of movement.

3.4. Total knee Arthroplasty with Deformity Correction (n=1)
A total knee arthroplasty was performed in a patient with severe varus deformity of the distal femur after a mal-union fracture treated non-operatively 30 years previously, with symptomatic osteoarthritis. A total knee arthroplasty with concurrent osteotomy was performed with deformity correction and stabilisation with dual Axsos distal femur plates and autologous bone grafting. The subject was pain-free with painless, stable range of movement of 70 degrees in his final follow-up.
3.5. Neutralising Stress Riser (n=1)
We had employed a distal femoral lateral Axsos plate in our patient with a severely arthritic knee with valgus deformity, where an ipsilateral total hip arthroplasty was in situ to prevent stress riser fractures due to the acute correction.
4. Discussion
Internal fixation for various scenarios occurring in knee arthroplasty have been reported in literature [3-7]. The aim of this study was to identify the various scenarios for which internal fixation was used during or within six weeks of the arthroplasty. Periprosthetic fractures around the knee are well documented and researched in literature and forms a distinct group, and therefore was not included in this case series. In our series of 8,453 primary knee arthroplasties between 2003 and 2018, we encountered 13 cases requiring internal fixations in the peri-operative period: five intra-operative fractures were immediately treated by performing internal fixation within the same surgery, five cases of occult fractures, diagnosed in the early post-operative period needing internal fixation, one case of TKA performed concurrently with a corrective osteotomy of the distal femur for distal femur malunion requiring bi condylar plating , one case was an osteoporotic insufficiency fracture of the proximal tibia before a scheduled elective TKA and one case where we used distal femur plate for neutralizing a stress riser in an inter-prosthetic construct.
4.1. Intra-Operative Fractures and Occult Fractures
Fractures occurring during primary knee arthroplasty are a rare complication of which limited literature is available. In our case series an incidence of 0.00058% has been found. Purudappa et al. found an incidence of 0.2-4.4% in a systematic review of 10 series that reported intra-operative fractures in primary knee arthroplasties [2]. Therefore 0.00058% seems a lot lower than the estimated incidence in literature. Risk factors for the occurrence of these fractures are osteoporosis, anterior cortical notching, rheumatoid arthritis, advanced age, female gender, chronic steroid use, metabolic bone disorder, posterior stabilization type of femoral implant (PS knee) and difficult surgical exposure due to severe deformities [2, 5, 8-10]. In our case series there was no history of confirmed osteoporosis nor chronic steroid use or metabolic bone disorder. A more female trend for intra-operative fractures was observed which aligns with the literature but could not be confirmed due to the small cohort.
In our series the mechanism that caused the fractures is thought to be the following: excessive sagittal saw cuts causing a fracture line along the medial tibial condyle, fracture during bony cuts and trial placement, excessive force while implanting the tibial tray, the keel cut with a standard saw being too deep, the tibial bone cut taken too medial and excessive force while implanting the tibial tray. Similar causes have been reported in literature [7, 11-13]. Measures to prevent these iatrogenic fractures were implemented in our institution such as using a toothbrush saw instead of the reciprocating saw for the keel cut. We also suggest the lateral cut of the tibial bone preparation in uni knees to be as close as possible to the medial border of the ACL. Judicious use of force while implanting is another remedial measure in prevention. Since the implementation of these measures in our institution, no intra-operative fracture has been documented. However, these measures for prevention need to be studied in a high-risk population group to confirm the efficacy of these measures. Insight in the mechanisms of these intra-operative fractures rise opportunities to prevent them in the future and therefore improve the outcome.
When it comes to internal fixation of these fractures, there are limited literature which addresses a superior type of internal fixation to address these fractures. Alden et al. proposed individual treatment strategies based on surgeon’s choice, bone quality and fracture pattern while using fracture fixation and arthroplasty principles in general [5]. Agarwala et al. treated tibial fractures with screws, sutures, or a combination of these [8]. Our observation suggests that longer locked plates, which offer a more robust buttress, seem to provide superior stability compared to smaller non-locking plates for a few reasons. Firstly, their extended length allows a greater contact area with the bone distributing the load over a larger surface and reducing stress concentration. This helps in preventing fractures or deformities. Secondly, the locking mechanism in these plates ensures a firmer connection between the plate and the bone, reducing micromotion and enhancing the overall structural integrity of the fixation. And finally, the increased rigidity provided by longer locked plates can better resist bending and torsional forces, which are common types of stress in orthopedic applications. This rigidity minimizes the risk of implant failure and promotes better bone healing.
Pinaroli et al. [6] reviewed primary, posterior stabilized (PS) total knee arthroplasties and reported a higher incidence of intraoperative fractures during the surgery, 40 intraoperative fractures in 1795 cases (2.2%). This case series investigated the various modalities of treatment of these fractures. Out of the total, the majority, comprising 27 cases (68%), were located on the tibial side, and were treated using a lengthy keel combined with an internal fixation device in the shape of an "8" made of metallic wire supported by two anteriorly positioned 4.5 mm diameter screws. These case series have suggested that intraoperative fractures are frequently encountered in posterior stabilized (PS) total knee replacements, with the most prevalent cause attributed to the box cut made during bone preparation.
Factors leading to such a complication can vary from technical errors such as excessive bone resection, fracture during bony and trial placement, excessive force used during implantation, and osteoporosis [4-6], though no patients in our series had a pre-operative or indeed post-operative diagnosis of osteoporosis.
4.2. Corrective Osteotomy
Angular deformities of the femur resulting from posttraumatic incidents can lead to deviations in the mechanical axis of the lower limb and improper alignment of the knee joint. Consequently, malalignment in the lower extremity may contribute to the development of knee osteoarthritis, which can eventually necessitate total knee arthroplasty (TKA). Achieving long- term success with TKA hinges on the accurate restoration of the mechanical axis and the equilibrium of soft tissues.
Osteotomies performed around the knee simultaneously with TKA are useful and often unavoidable in regaining a proper alignment of the lower limb in these cases.These realignment osteotomy for extra articular correction of the deformity with osteoarthritis of knee is another indication of concurrent use of fixation devices in knee arthroplasty .The osteotomies should be planned well in advance and taking into consideration the principles of deformity correction. Key points to consider is the magnitude and distance of deformity to the joint line which will determine the extent of bone resection and the optimal balance of soft tissues for a functional TKA as suggested by Wolff et al. [14]. A coronal plane deformity of more than ten degrees and sagittal plane deformity of more than twenty degrees and a deformity far from the joint (>10cm) entails an extra articular correction [15, 16]. Fixation option should be selected with consideration of soft tissues around the knee & the degree of femoral bone resection [17].We report one case of staged TKA following corrective osteotomy for extra articular correction of a post traumatic varus malunion deformity of the distal femur with osteoarthritis of knee in this series.
The choice of fixation method should consider the condition of the soft tissues surrounding the knee and the extent of femoral bone resection. To ensure precise anatomical alignment and secure stabilization at the osteotomy site, we opted for the use of locked periarticular plates. We employed two plates in this case, as the condyles split during the intraoperative procedure.
4.3. Stress Neutralization in Inter-Prosthetic Constructs
The increasing use of implants in orthopedics has led to the predisposition for stress riser fractures. Cortical defects create a stress concentration. Therefore, surgical care and consideration are needed during and after surgery. Choosing a very hard implant is not good for a patient with weak bones. Performing surgery to reduce stress concentration at the end of implants in the intramedullary and extra-medullary bone is a good way to avoid stress risers. Obvious stress riser fractures are best managed by secure internal fixation and early ambulation. There are several compelling reasons for this approach. Firstly, secure internal fixation methods are essential in stabilizing the fractured bone segments. Without this stable fixation, the fracture may fail to heal properly or could deteriorate, leading to potential complication [5].
Additionally, this approach promotes the healing process. By providing secure fixation, it ensures that the bone ends are maintained in the correct position, facilitating better alignment, and ultimately enhancing the healing process. Furthermore, the strategy of secure internal fixation reduces the risk of non-union. Non-locked plating was associated with an 11.9 times higher risk for nonunion when compared with locked plating in the treatment of inter-prosthetic femur fractures [18]. Another key advantage of this approach is the potential for a faster recovery.
Negating the stress riser as a ‘neutralization plate’ is another important use of internal fixation device in knee arthroplasty [19, 20]. It is known that intervening bone in inter-prosthetic constructs are prone for fracture load. Biomechanical studies of the same are confusing at times [19-21]. It is postulated that, a fracture will most likely originate at the lateral side of the inter-prosthetic gap, where high tensile stresses will occur [21]. Factors influencing stress riser severity are gap distance, ‘loose prosthesis’ increasing the stress in the intervening area, modality chosen to mitigate such forces, e.g. intramedullary nail, distal femur plate, orthogonal plating etc. [19, 22]. Lehmann et al. suggested decreasing the lateral inter-prosthetic distance as one of the ways of mitigating stress riser [19]. We had employed a distal femoral lateral Axsos plate in our patient with a severely arthritic knee with valgus deformity, where an ipsilateral total hip arthroplasty was in situ. To prevent stress risers due to the acute correction, we performed a distal lateral femur plating concurrently with knee arthroplasty.
Our series confirms a lower incidence of perioperative fractures, lower than previously recorded in literature, particularly in our TKR patients .When encountered, the surgeon should be adept in dealing with these problems and internal fixation sets and implants should ideally be available for this eventuality. Our case series may not yield conclusive evidence on the usage of specific types of internal fixation device due to the limited number of cases, however the use of the locked plates does seem to be robust, with a high chance of progression to union and low risk of loss of reduction, internal fixation failure or metalwork prominence. We don’t have enough data to comment on the impact of fixative on longevity of the arthroplasty. The use of locked plates has several potential biomechanical advantages in stabilizing mainly metaphyseal fractures with often limited screw distances due to the presence of other implants and lowers the risk of potentially troublesome screw back-out.
This series demonstrates the use of a range of internal fixation devices in several potential scenarios requiring its use, some of which have not been previously reported, ranging from stabilizing an avulsion to undertaking a single stage realignment osteotomy and total knee replacement. It would seem pertinent that arthroplasty surgeons, or at least 1 member of a group, maintain their surgical skills to undertake this type of internal fixation surgery or to utilize a colleague with these skills when needed and that appropriate internal fixation kit and implants are available for these rare occurrences.
Weaknesses of this study are the small cohort of cases, as well as lack of identification of confounding factors in the incidence of fractures.
5. Conclusion
A small percent of patients requires acute, internal fixation techniques during or shortly after primary knee arthroplasty. Our study suggests the overall incidence of early peri-prosthetic fractures is lower (0.001%) compared with historic data. Patient and technique factors are implicated in causation of these fractures.Treating surgeons should understand the biomechanical principles and consequences of fixation constructs when faced with the problem of treating such complex primary knee arthroplasty cases ,with lessons gained also being applicable to revision total knee situations.A sound knowledge of fracture fixation and retaining the skillset for internal fixation is essential in these situations. Locking plate constructs in conjunction with stemmed arthroplasty implants appear to be effective in this patient group.
Ethics Approval and Consent to Participate
All procedures in studies involving human participants were in accordance with the ethical standards of the institutional research committee at which the studies were conducted (IRB approval number 93/2012/U/Oss) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflicts of Interest
None.
Competing Interests
None.
Funding
None.
Author’s Contributions
Conception and design: Mr. Sunny Deo. Acquisition of data: Mr. Sunny Deo, Mr. Vinayak Venugopal. Drafting of the manuscript: Mr. Vinayak Venugopal. Critical revision of the manuscript for important intellectual content: Mr. Sunny Deo. Administrative, technical, or material support: Mr. Vinayak Venugopal. Supervision: Mr. Sunny Deo.
Availability of Supporting Data
Not applicable.
Acknowledgments
None.
REFERENCES
[1] G
S Matharu, D J Culliford, A W Blom, et al. “Projections for primary hip and
knee replacement surgery up to the year 2060: an analysis based on data from
The National Joint Registry for England, Wales, Northern Ireland and the Isle
of Man.” Ann R Coll Surg Engl, vol. 104, no. 6, pp. 443-448, 2022. View
at: Publisher Site | PubMed
[2] Prabhudev
Prasad Purudappa, Sruthi Priyavadhana Ramanan, Sujit Kumar Tripathy, et al.
“Intra-operative fractures in primary total knee arthroplasty - a systematic
review.” Knee Surg Relat Res, vol. 32, no. 1, pp. 40, 2020. View at: Publisher Site | PubMed
[3] Jae
Doo Yoo, Nam Ki Kim “Periprosthetic fractures following total knee
arthroplasty.” Knee Surg Relat Res, vol. 27, no. 1, pp. 1-9, 2015. View
at: Publisher Site | PubMed
[4] G
A Engh, D J Ammeen “Periprosthetic fractures adjacent to total knee implants:
treatment and clinical results.” Instr Course Lect, vol. 47, pp.
437-448, 1998. View at: PubMed
[5] Kris
J Alden, William H Duncan, Robert T Trousdale, et al. “Intraoperative fracture
during primary total knee arthroplasty.” Clin Orthop Relat Res, vol.
468, no. 1, pp. 90-95, 2010. View at: Publisher Site | PubMed
[6] A
Pinaroli, S R Piedade, E Servien, et al. “Intraoperative fractures and ligament
tears during total knee arthroplasty A. 1795 posterostabilized TKA continuous
series.” Orthop Traumatol Surg Res, vol. 95, no. 3, pp. 183-189, 2009.
View at: Publisher Site | PubMed
[7] J.
B. Seeger, D. Haas, S. Jäger, et al. “Extended sagittal saw cut significantly
reduces fracture load in cementless unicompartmental knee arthroplasty compared
to cemented tibia plateaus: an experimental cadaver study.” Knee Surg Sports
Traumatol Arthrosc, vol. 20, no. 6, pp. 1087-1091, 2012. View at: Publisher Site | PubMed
[8] Sanjay
Agarwala, Supreet Bajwa, Mayank Vijayvargiya “Intra- operative fractures in
primary Total Knee Arthroplasty.” J Clin Orthop Trauma, vol. 10, no. 3,
pp. 571-575, 2019. View at: Publisher Site | PubMed
[9] A
Pinaroli, S R Piedade, E Servien, et al. “Intraoperative fractures and ligament
tears during total knee arthroplasty. A 1795 posterostabilized TKA continuous
series.” Orthop Traumatol Surg Res, vol. 95, no. 3, pp. 183-189, 2009.
View at: Publisher Site | PubMed
[10]
Alex H F Pun, Wai-Ki Pun, Peter
Storey “Intra-operative fracture in posterior-stabilised total knee
arthroplasty.” J Orthop Surg (Hong Kong), vol. 23, no. 2, pp. 205-208,
2015. View at: Publisher Site | PubMed
[11]
D W Murray, J W Goodfellow, J J
O'Connor “The Oxford medial unicompartmental arthroplasty (a ten year survival
study).” J Bone Joint Surg Br, vol. 80, no. 6, pp. 983-989, 1998. View
at: Publisher Site | PubMed
[12]
Grzegorz Rudol, Mark P Jackson,
Stephen E James “Medial tibial plateau fracture complicating unicompartmental
knee arthroplasty.” J Arthroplast, vol. 22, no. 1, pp. 148-150, 2007.
View at: Publisher Site | PubMed
[13]
Hemant Pandit, David W Murray,
Christopher A F Dodd, et al. “Medial tibial plateau fracture and the Oxford
unicompartmental knee.” Orthopedics, vol. 30, no. 5 Suppl, pp. 28-31,
2007. View at: PubMed
[14]
A M Wolff, D S Hungerford, C L Pepe
“The effect of extraarticular varus and valgus deformity on total knee
arthroplasty.” Clin Orthop Relat Res, no. 271, pp. 35-51, 1991. View at:
PubMed
[15]
Jun-Wen Wang, Ching-Jen Wang “Total
knee arthroplasty for arthritis of the knee with extra-articular deformity.” J
Bone Joint Surg Am, vol. 84, no. 10, pp. 1769-1774, 2002. View at: Publisher Site | PubMed
[16]
J H Lonner, J M Siliski, P A Lotke
“Simultaneous femoral osteotomy and total knee arthroplasty for treatment of
osteoarthritis associated with severe extra articular deformity.” J Bone
Joint Surg Am, vol. 82, no. 3, pp. 342-348, 2000. View at: Publisher Site | PubMed
[17]
Ashok Rajgopal, Attique Vasdev, Vivek
Dahiya, et al. “Total knee arthroplasty in extra articular deformities: a
series of 36 knees.” Indian J Orthop, vol. 47, no. 1, pp. 35-39, 2013.
View at: Publisher Site | PubMed
[18]
Karl Stoffel, Christoph Sommer,
Vasiliki Kalampoki, et al. “The influence of the operation technique and
implant used in the treatment of periprosthetic hip and interprosthetic femur
fractures: a systematic literature review of 1571 cases.” Arch Orthop Trauma
Surg, vol. 136, no. 4, pp. 553-561, 2016. View at: Publisher Site | PubMed
[19]
Wolfgang Lehmann, Martin Rupprecht,
Nils Hellmers, et al. “Biomechanical evaluation of peri- and interprosthetic
fractures of the femur.” J Trauma, vol. 68, no. 6, pp. 1459-1463, 2010.
View at: Publisher Site | PubMed
[20]
Wolfgang Lehmann, Martin Rupprecht,
Jacob Nuechtern, et al. “What is the risk of stress risers for interprosthetic
fractures of the femur? A biomechanical analysis.” Int Orthop, vol. 36,
no. 12, pp. 2441-2446, 2012. View at: Publisher Site | PubMed
[21] Thomas Quirynen, Kristoff Corten, Olivier Segal, et al. “Small interprosthetic gaps do not increase femoral peri-prosthetic fracture risk. An in vitro biomechanical analysis.” Acta Orthop Belg, vol. 83, no. 2, pp. 197-204, 2017. View at: PubMed
[22] Christiaan N Mamczak, Michael J Gardner, Brett Bolhofner, et al. “Interprosthetic femur fractures.” J Orthop Trauma, vol. 24, no. 12, pp. 740-744, 2010. View at: Publisher Site | PubMed
